Introduction
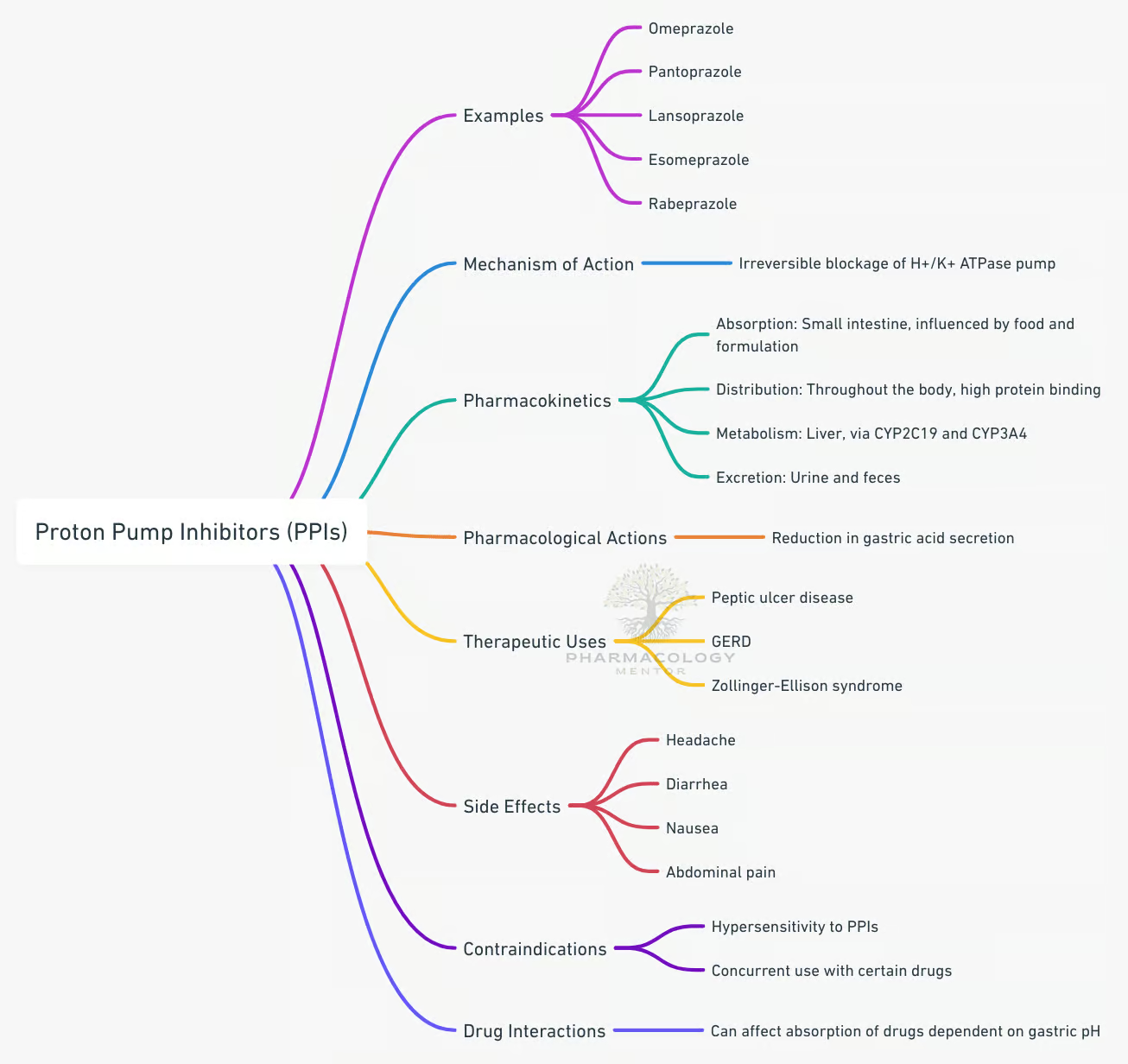
Proton pump inhibitors (PPIs) have revolutionized the management of acid-related gastrointestinal (GI) disorders by rendering potent and long-lasting suppression of gastric acid secretion. Introduced in the late twentieth century, PPIs—exemplified by omeprazole, lansoprazole, pantoprazole, rabeprazole, esomeprazole, and dexlansoprazole—effectively mitigate gastric hyperacidity, enabling healing of peptic ulceration and alleviation of reflux symptoms (Katzung, 2020). Used extensively for indications ranging from peptic ulcer disease (PUD) and gastroesophageal reflux disease (GERD) to prophylaxis against stress-related mucosal damage, these medications rank among the most commonly prescribed drugs globally.
- Introduction
- Biology of Gastric Acid Secretion
- Mechanism of Action of Proton Pump Inhibitors
- Classification and Available Agents
- Pharmacokinetics of Proton Pump Inhibitors
- Clinical uses of Proton Pump Inhibitors
- Adverse Effects of Proton Pump Inhibitors
- Drug Interactions
- PPIs in Special Populations
- Optimizing Proton Pump Inhibitor Therapy
- Long-Term Safety Concerns
- Managing PPI-Associated Complications
- Comparative Efficacy and Practical Selection
- Future Developments
- Clinical Pearls and Best Practices
- Conclusion
- References (Book Citations)
Despite their broad acceptance, proton pump inhibitors demand judicious usage. This review explores the pharmacology of PPIs, encompassing their mechanism of action, pharmacokinetics, clinical applications, adverse effects, drug interactions, and best practices for optimizing therapy. Sources are drawn from “Goodman & Gilman’s The Pharmacological Basis of Therapeutics,” “Katzung BG, Basic & Clinical Pharmacology,” and “Rang & Dale’s Pharmacology,” which offer foundational insights.
Biology of Gastric Acid Secretion
Anatomy and Physiology of the Stomach
Gastric acid production primarily occurs in the parietal cells located in the fundus and body of the stomach. These specialized cells harbor the H⁺/K⁺-ATPase—commonly referred to as the proton pump—which actively secretes hydrogen ions into the gastric lumen in exchange for potassium ions.
Acid Secretory Regulation
Gastric acid secretion follows a complex regulation influenced by three key factors (Goodman & Gilman, 2018):
- Acetylcholine (ACh) release from enteric neurons, stimulating M3 receptors on parietal cells.
- Histamine from enterochromaffin-like (ECL) cells, acting on H₂ receptors.
- Gastrin from G cells, triggering both direct parietal cell stimulation and histamine release from ECL cells.
Once these signals converge, the final step of acid secretion is mediated by the H⁺/K⁺-ATPase pump on the parietal cell canalicular membrane. Proton pump inhibitors irreversibly inhibit this pump, thereby suppressing gastric acid secretion irrespective of the underlying stimulus (Rang & Dale, 2019).
Mechanism of Action of Proton Pump Inhibitors
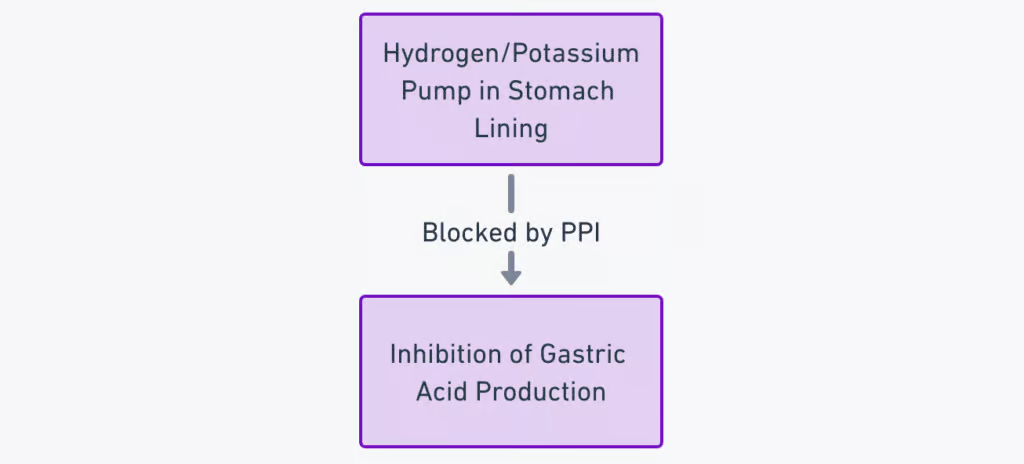
Proton pump inhibitors are weak bases that, upon entering the systemic circulation, travel to the parietal cells and accumulate in the acidic canaliculi. As prodrugs, they become activated by protonation in the acidic environment and undergo a molecular rearrangement to yield the active sulfenamide moiety. This intermediate permanently binds to the cysteine residues on the H⁺/K⁺-ATPase, forming a covalent (disulfide) bond (Katzung, 2020). Consequently, the pump is rendered inactive.
Because PPIs irreversibly inhibit the enzyme, acid secretion can only resume as the parietal cells synthesize new proton pumps—a process typically requiring ~3 to 5 days. As a result, PPIs provide long-lasting suppression of gastric acid production. The clinical end result is a significant and prolonged reduction in gastric acidity, fostering ulcer healing and alleviating acid reflux symptoms (Goodman & Gilman, 2018).
Classification and Available Agents
First-Generation
- Omeprazole: The prototype PPI.
- Lansoprazole: Formulated to offer a similar potency profile.
Second-Generation/Enantiomeric Compounds
- Esomeprazole: The S-isomer of omeprazole, potentially offering more consistent acid suppression in some patients.
- Dexlansoprazole: R-enantiomer of lansoprazole, featuring a dual delayed-release formulation for extended effect (Rang & Dale, 2019).
Other PPIs
- Pantoprazole
- Rabeprazole
All PPIs share a similar basic core structure but exhibit minor pharmacokinetic differences—particularly in metabolism and half-life. These differences can impact drug interactions and, for certain patients, clinical efficacy (Katzung, 2020).
Pharmacokinetics of Proton Pump Inhibitors
Absorption
PPIs are acid-labile, necessitating administration in enteric-coated formulations to protect them from gastric acid degradation. They are absorbed primarily in the small intestine, typically reaching peak plasma concentrations within 2–3 hours (Goodman & Gilman, 2018).
Distribution
Following absorption, PPIs diffuse into parietal cell canaliculi where the pH is substantially lower, prompting prodrug activation. Because they bind covalently with the proton pump, the site-specific targeting leads to extended durations of action despite relatively short plasma half-lives (Rang & Dale, 2019).
Metabolism and Elimination
- Hepatic Metabolism: PPIs undergo extensive metabolism in the liver—most commonly via CYP2C19 and CYP3A4 pathways.
- Short Plasma Half-life: Typically 1–1.5 hours, but acid suppression persists for ~24 hours or more.
- Interindividual Variation: Genetic polymorphisms in CYP2C19 can influence PPI clearance and efficacy (Katzung, 2020).
- Renal Excretion: Inactive hepatic metabolites are excreted via the kidney.
Dosing Considerations
- Once-Daily Administration: Commonly recommended, often before the first meal of the day, to match peak proton pump activity.
- Twice-Daily: Sometimes indicated for refractory GERD or hypersecretory conditions (e.g., Zollinger-Ellison syndrome).
- Immediate vs. Delayed Release: Dexlansoprazole employs a dual delayed-release system, providing a prolonged plasma concentration (Goodman & Gilman, 2018).
Clinical uses of Proton Pump Inhibitors
Peptic Ulcer Disease (PUD)
- Duodenal Ulcers: Typically heal within 4 weeks of once-daily PPI therapy.
- Gastric Ulcers: May require slightly extended treatment duration (6–8 weeks). PPIs foster faster healing rates compared to H₂ receptor antagonists.
- H. pylori Eradication: Triple therapy (PPI + clarithromycin + amoxicillin/metronidazole) or quadruple therapy often used. PPIs raise intragastric pH, enhancing antibiotic efficacy (Katzung, 2020).
Gastroesophageal Reflux Disease (GERD)
Proton pump inhibitors represent the gold-standard therapy for both erosive esophagitis and long-term management of moderate-to-severe GERD symptoms. Their profound acid suppression aids in mucosal healing and symptom relief, outperforming H₂ antagonists. On-demand or step-down strategies may be considered in mild cases (Rang & Dale, 2019).
Erosive Esophagitis and Barrett’s Esophagus
In severe erosive disease, PPIs accelerate mucosal healing, reduce complications such as strictures, and may limit further progression. Though the data regarding Barrett’s esophagus regression remain variable, PPIs are integral to controlling underlying acid reflux (Goodman & Gilman, 2018).
Stress-Related Mucosal Damage
Critically ill patients (in ICU settings) often receive PPIs for prophylaxis against stress-related ulcerations. While earlier regimens included antacids or sucralfate, PPIs have largely become the first-line prophylactic agents. However, clinicians balance the potential benefits against infection risks (Katzung, 2020).
Zollinger-Ellison Syndrome (ZES)
This gastrinoma-driven hypersecretory condition produces massive acid outputs, leading to recurrent peptic ulcers. High-dose or frequent PPI dosing effectively suppresses acid production, mitigating ulcerative complications (Rang & Dale, 2019).
Additional Indications
- Non-ulcer Dyspepsia: Empirical PPI trials are sometimes used for persistent reflux symptoms.
- Prevention of Bleeding from NSAID-Associated Ulcers: Especially in patients at high GI risk continuing NSAID therapy, concomitant PPI use drastically reduces ulceration risk (Goodman & Gilman, 2018).
Adverse Effects of Proton Pump Inhibitors
Gastrointestinal and Nutritional Considerations
- Impacted Nutrient Absorption: Long-term PPI therapy can impair absorption of vitamin B12, iron, calcium, and magnesium. Achlorhydria (lack of stomach acid) compromises the release of these micronutrients from dietary proteins (Katzung, 2020).
- Hypomagnesemia: Chronic use occasionally leads to severe magnesium deficiency, potentially causing neuromuscular irritability.
- Fracture Risk: Reduced calcium absorption and possible direct effects on bone remodeling raise concerns about osteoporosis and fracture risk, particularly with prolonged therapy (Rang & Dale, 2019).
Infections
- Clostridioides difficile-Associated Diarrhea (CDAD): Decreased gastric acidity can permit bacterial overgrowth or survivability, increasing the likelihood of C. difficile infection.
- Community-Acquired Pneumonia: Some epidemiological links have emerged, although confounding factors exist.
Potential Renal Complications
- Acute Interstitial Nephritis (AIN) has been reported with PPIs (rare but serious). Prompt drug discontinuation is crucial upon suspicion.
- Chronic Kidney Disease (CKD) risk may be slightly elevated in users of long-term PPI therapy, though causality remains debated (Goodman & Gilman, 2018).
Neurological and Cardiovascular Effects
- Rebound Hyperacidity upon abrupt PPI withdrawal can exacerbate symptoms of reflux. A step-down taper may mitigate rebound phenomena (Katzung, 2020).
- Possible Dementia Risk: Observational studies suggest an association, but causative links are not definitively confirmed.
- Cardiovascular Effects: Generally minimal. However, the potential for PPIs (especially omeprazole) to interfere with clopidogrel activation raises concerns about stent thrombosis (Rang & Dale, 2019).
Other Side Effects
- Headache, nausea, diarrhea are relatively common mild complaints.
- Allergic Reactions: Rare, but urticarial or anaphylactic events can occur.
- Subacute Myopathy (extremely uncommon) (Goodman & Gilman, 2018).
Drug Interactions
Cytochrome P450 Metabolism
- Omeprazole and esomeprazole can inhibit CYP2C19, affecting clearance of diazepam, phenytoin, and others.
- Clopidogrel requires CYP2C19 for bioactivation; concurrent use with certain PPIs (especially omeprazole) may reduce clopidogrel’s antiplatelet effect. Current guidelines recommend caution, possibly preferring pantoprazole (Katzung, 2020).
Drugs Sensitive to Gastric pH
By elevating gastric pH, PPIs may alter the absorption of certain drugs reliant on acidic conditions. For instance:
- Ketoconazole, itraconazole: Reduced absorption in less acidic environments.
- Digoxin, certain iron salts: May see altered absorption (Rang & Dale, 2019).
Other Key Interactions
- Methotrexate: PPIs, particularly omeprazole, can hamper renal clearance of high-dose methotrexate, prompting toxicity.
- HIV Protease Inhibitors (e.g., atazanavir) and PPIs: Potential for decreased antiretroviral efficacy due to reduced solubility in higher pH (Goodman & Gilman, 2018).
PPIs in Special Populations
Pediatric Patients
PPIs can be employed for GERD, erosive esophagitis, or refractory acid-related disorders in children. Dosing regimens are weight-based. Despite generally good tolerance, vigilance against infection risk (e.g., respiratory or GI) is warranted (Katzung, 2020).
Geriatric Populations
Older adults are more prone to the complications of PPIs, including fractures, electrolyte disturbances, and infection risks. Reduced dosing and close monitoring of bone health and renal function are prudent (Goodman & Gilman, 2018).
Patients with Liver Disease
Because PPIs undergo hepatic metabolism, severe liver disease might impair clearance. Dose adjustments or selection of PPIs with minimal hepatic metabolism (e.g., rabeprazole) may be considered (Rang & Dale, 2019).
Pregnancy and Lactation
PPIs are designated generally as Category B or C (depending on the specific agent). Omeprazole and lansoprazole have relatively longer safety track records, although non-drug measures or short-term H₂ antagonists are often tried first if feasible. Lactational excretion is minimal, but caution is advised as a general principle (Katzung, 2020).
Optimizing Proton Pump Inhibitor Therapy
Timing of Administration
- Pre-breakfast Dosing: PPIs are most effective when taken ~30 minutes before the first meal, because parietal cells are actively synthesizing acid pumps after a nocturnal fast.
- Twice-Daily: Indicated in certain refractory cases or hypersecretory states (Goodman & Gilman, 2018).
Treatment Duration
- Uncomplicated GERD: 4–8 weeks, often sufficient to achieve healing. Maintenance therapy follows if relapse occurs frequently.
- Peptic Ulcer: Typically 4 weeks for duodenal ulcers, 6–8 weeks for gastric ulcers.
- Zollinger-Ellison Syndrome: Long-term, high-dose therapy is often required, guided by acid output monitoring (Rang & Dale, 2019).
Step-Down / On-Demand Approaches
- Step-Down: Initiate higher-intensity therapy (e.g., standard once-daily PPI) and attempt to reduce the dose or frequency once symptom control is achieved, minimizing adverse effects and cost.
- On-Demand: In mild, intermittent GERD, patients may resume a PPI for brief courses during symptomatic episodes (Katzung, 2020).
Combination with Other Agents
- Antibiotics and Bismuth: For H. pylori eradication.
- Prokinetics (e.g., metoclopramide) in severe refractory GERD or gastroparesis.
- Mucosal Protectants (e.g., sucralfate) if needed for stress ulcer prophylaxis or additional ulcer coverage (Goodman & Gilman, 2018).
Long-Term Safety Concerns
Chronic Kidney Disease and Hypomagnesemia
Persistent PPI use has been epidemiologically linked with a higher incidence of CKD. While causality remains unconfirmed, clinicians should monitor renal function in patients on prolonged therapy. Furthermore, serum magnesium checks are warranted if muscle cramps, palpitations, or seizures arise (Rang & Dale, 2019).
Bone Health
Fracture risk (e.g., hip or spine) becomes more pertinent with therapy extending beyond a year. Ensuring adequate calcium and vitamin D intake and encouraging weight-bearing exercise can be beneficial. If feasible, limiting PPI therapy or applying step-down strategies mitigates risks (Katzung, 2020).
Clostridioides difficile Infections
Reducing gastric acidity inadvertently fosters a less hostile environment for pathogens, facilitating colonization. Particularly in hospitalized or compromised individuals, antibiotic usage in conjunction with PPI therapy elevates the risk of C. difficile overgrowth (Goodman & Gilman, 2018).
Gastric Carcinoid Tumors
After longtime acid suppression, serum gastrin levels can rise, potentially spurring enterochromaffin-like (ECL) cell hyperplasia. However, the clinical significance for gastric carcinoid formation in humans is still uncertain, with few documented cases (Rang & Dale, 2019).
Managing PPI-Associated Complications
De-escalating Therapy
When clinically appropriate, stepping down or discontinuing PPIs may reduce unwanted consequences. A gradual taper over 2–4 weeks helps avert rebound hyperacidity, which can mimic relapse of GERD or ulcer symptoms (Katzung, 2020).
Monitoring Electrolytes and Bone Density
- Serum Magnesium: Periodic checks, especially in cases of arrhythmias, neuromuscular excitability, or prolonged QT.
- Bone Density: For patients on multi-year therapy, dual-energy X-ray absorptiometry (DXA) screening may be prudent (Goodman & Gilman, 2018).
Infection Control
- Appropriate Antibiotic Stewardship: Minimizing overlapping or unnecessary antibiotic therapy in patients on PPIs.
- Clinical Vigilance: Early recognition of C. difficile–associated diarrhea (ongoing watery stools, abdominal pain, labile temperature) triggers prompt testing and intervention (Rang & Dale, 2019).
Comparative Efficacy and Practical Selection
Despite minor variations in half-life, metabolism, and potential for drug interactions, all PPIs generally demonstrate comparable efficacy when used at equipotent doses (Katzung, 2020). Differences often revolve around:
- Cost: Some older agents (e.g., generic omeprazole) are much cheaper.
- Pharmacogenetics: In poor metabolizers of CYP2C19, omeprazole or esomeprazole might provide more stable plasma levels.
- Clinically Significant Interactions: For patients on clopidogrel, some guidelines favor pantoprazole due to fewer CYP2C19 interactions (Rang & Dale, 2019).
Future Developments
Novel PPIs and Potassium-Competitive Acid Blockers (PCABs)
Potassium-competitive acid blockers (PCABs)—like vonoprazan—inhibit the proton pump via reversible binding to the K⁺ site, potentially offering more rapid and consistent acid suppression. Used increasingly in parts of Asia, these agents await broader global adoption pending further research (Goodman & Gilman, 2018).
Extended-Release Formulations
Advanced formulations aim for more flexible dosing (e.g., dual-releasedexlansoprazole) or shorter onsets (e.g., combination with sodium bicarbonate). The quest for agents that circumvent PPI limitations continues.
Personalized Medicine
Pharmacogenomic profiling of CYP2C19 variants might guide the choice or dose adjustments of PPIs. Individuals with ultra-rapid metabolism may require higher or more frequent dosing, whereas poor metabolizers might do well on standard or reduced doses (Katzung, 2020).
Clinical Pearls and Best Practices
- Confirm Indication: Use PPIs only where indicated (e.g., documented GERD, peptic ulcer, high GI risk). Unnecessary prescribing fosters side effects and cost.
- Short-Term Trials: For mild GERD, limit PPI duration to 4–8 weeks. Reassess the need after symptom resolution.
- Assess for H. pylori: If ulcer disease is present, evaluate for H. pylori and eradicate if positive.
- Counsel on Administration: Advise patients to take PPIs in the morning, 30 minutes before breakfast, for optimal effect.
- Monitor for Nutritional Deficiencies: In long-term users, check B12, magnesium, and ensure adequate calcium/vitamin D intake (Rang & Dale, 2019).
- Avoid Abrupt Withdrawal: Taper in cases of prolonged therapy to prevent rebound acid hypersecretion.
- Mind Drug Interactions: Notably with clopidogrel, methotrexate, and certain antifungals/antiretrovirals.
- Use Alternatives Where Possible: For minor dyspepsia or short-term reflux, an H₂-blocker or antacid might suffice (Katzung, 2020).
Conclusion
Proton pump inhibitors have reshaped acid-related disease therapy, offering potent and sustained suppression of gastric acid secretion. Their application spans peptic ulcer disease, GERD, stress ulcer prophylaxis, and rare hypersecretory syndromes like Zollinger-Ellison. By irreversibly inhibiting the H⁺/K⁺-ATPase, PPIs deliver robust efficacy yet invite caution regarding long-term safety issues—ranging from malabsorption (B12, magnesium) to osteoporosis and infection risks.
Clinicians can maximize the benefit-risk profile of PPIs by prescribing them thoughtfully, employing the lowest effective dose for the shortest duration necessary, and monitoring for nutrient deficiencies or renal issues. Emerging PCABs and advanced formulations hint at the next wave of acid-suppressive therapeutics, although further trials are needed to confirm their relative advantages. Ultimately, patient-specific factors—comorbidities, concurrent medications, genetic polymorphisms—guide the choice, dosing, and duration of proton pump inhibitors in modern clinical practice (Goodman & Gilman, 2018; Katzung, 2020; Rang & Dale, 2019).
References (Book Citations)
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- Katzung BG, Basic & Clinical Pharmacology, 14th Edition.
- Rang HP, Dale MM, Rang & Dale’s Pharmacology, 8th Edition.









[…] Proton Pump Inhibitors […]
[…] Proton pump inhibitors: Concurrent use with H2 receptor antagonists may reduce the effectiveness of both drugs. […]