Introduction
Magnesium is the fourth most abundant cation in the human body and plays a critical role in numerous physiological processes. Magnesium sulfate (MgSO4) is an inorganic salt that has been used medicinally for over a century to treat a variety of conditions. This chapter will provide an overview of the pharmacology of magnesium sulfate, including its mechanism of action, pharmacokinetics, indications and uses, dosing, adverse effects, and drug interactions.
Chemical Structure and Properties
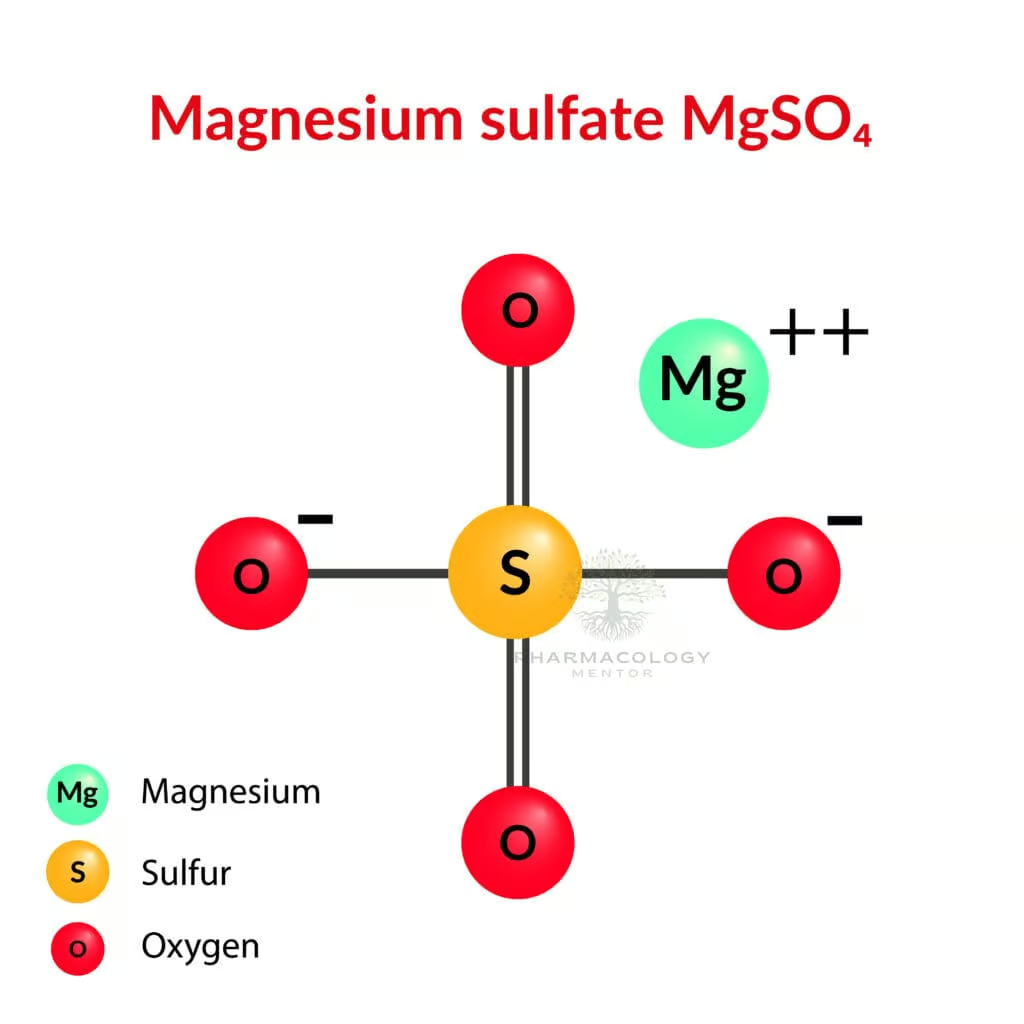
Magnesium sulfate has the molecular formula MgSO4 and a molar mass of 120.37 g/mol. It is a white crystalline solid at room temperature that is highly soluble in water. An aqueous solution of magnesium sulfate has a pH of around 6.0 to 7.5. Magnesium sulfate is available in various pharmaceutical formulations, including injectable solutions, orally disintegrating tablets, and topical gels and creams.
Mechanism of Action
The pharmacological effects of magnesium are primarily due to its role as a cofactor for over 300 enzymatic reactions and its ability to modulate ion channels. Magnesium acts as a physiological calcium channel blocker and induces smooth muscle relaxation. It decreases the release of acetylcholine from motor nerve terminals and reduces the sensitivity of post-junctional membranes, resulting in neuromuscular blockade. Magnesium also acts as an N-methyl-D-aspartate (NMDA) receptor antagonist in the central nervous system.
The mechanism behind magnesium’s neuroprotective and anticonvulsant properties likely involves antagonism of excitatory amino acids and inhibition of NMDA-mediated calcium influx into neurons. Magnesium inhibits calcium entry through voltage-gated channels, which contributes to its antiarrhythmic effects. It also enhances the activity of parathyroid hormone and plays a role in bone homeostasis.
Pharmacokinetics
Magnesium sulfate can be administered intravenously, intramuscularly, or orally. Oral bioavailability is limited due to poor absorption from the gastrointestinal tract. When given intravenously, the onset of action occurs within minutes, and effects persist for 30 minutes after the infusion is stopped.
About 30–50% of total body magnesium is located in bones, with the remainder in soft tissues. Less than 1% of total body magnesium is located in the blood, with normal serum concentrations ranging from 1.5 to 2.5 mEq/L. Serum magnesium levels do not always correlate with total body stores. Approximately 20–30% of serum magnesium is bound to proteins, primarily albumin.
Magnesium is eliminated almost entirely by the kidneys, with 95% of the filtered load reabsorbed under normal conditions. Renal magnesium excretion is increased in the setting of hypermagnesemia, hypercalcemia, volume expansion, metabolic acidosis, and in response to diuretics and other drugs. The half-life of intravenous magnesium sulfate is approximately 4 hours in patients with normal renal function. Significant accumulation can occur with repeated dosing in renal impairment.
Clinical Indications and Uses
- Eclampsia and preeclampsia: Magnesium sulfate is the drug of choice for preventing and controlling seizures associated with severe preeclampsia and eclampsia. It is typically administered as a 4-6 g IV loading dose followed by a continuous infusion of 1-2 g/hr.
- Torsades de pointes: Intravenous magnesium sulfate (1-2 g IV push) is used to terminate episodes of torsades de pointes, a potentially life-threatening form of polymorphic ventricular tachycardia associated with QT prolongation. Magnesium is the treatment of choice even if the serum magnesium concentration is within the normal range.
- Asthma: Intravenous magnesium sulfate is used as an adjunct to standard therapy in patients with acute severe asthma who have not responded to inhaled bronchodilators and corticosteroids. The typical dose is 2 g infused over 20 minutes.
- Tetanus: Magnesium sulfate is sometimes used as an adjunct to benzodiazepines and neuromuscular blockers to control muscle spasms in severe tetanus. Doses of 40 mg/kg/day or higher may be required, with careful monitoring of serum levels and deep tendon reflexes.
- Constipation: Oral magnesium salts (typically magnesium hydroxide or magnesium citrate) are commonly used as osmotic laxatives for the relief of occasional constipation. They work by drawing water into the intestinal lumen.
- Dyspepsia and gastroesophageal reflux: Magnesium is a component of some over-the-counter antacids used for the relief of heartburn and indigestion. Magnesium hydroxide and magnesium trisilicate are common ingredients.
- Magnesium deficiency: Though true symptomatic magnesium deficiency is uncommon, it can occur due to inadequate intake, excessive losses (diarrhoea, vomiting), or impaired absorption. Oral magnesium salts may be used for supplementation, but parenteral magnesium may be necessary in severe cases.
Dosage and Administration
The dosage of magnesium sulfate varies depending on the indication, route of administration, and individual patient factors such as age, weight, and renal function. Some general principles:
- For the treatment of eclampsia/preeclampsia: 4-6 g loading dose over 20–30 min, followed by 1-2 g/hr continuous infusion. Aim to keep serum levels 4-7 mEq/L.
- For torsades de pointes: 1-2 g IV push over 1-2 min, may repeat in 10-15 min if needed.
- For severe asthma: 2 g IV infusion over 20 min. Some studies have used repeat doses q30min for a total of 3 doses.
- For supplementation in deficiency: Oral dosing varies, but typically 300–600 mg/day of elemental magnesium in divided doses. Parenteral dosing depends on serum levels.
Adverse Effects and Precautions
The most common adverse effects of magnesium sulfate are flushing, sweating, and a sense of warmth, especially with rapid intravenous administration. Nausea, vomiting, and diarrhoea are possible with oral ingestion. Hypermagnesemia can cause hypotension, muscle weakness, fatigue, potentially life-threatening respiratory depression and paralysis, cardiac conduction abnormalities, and arrest.
Magnesium should be used with caution in patients with myasthenia gravis or other disorders of neuromuscular transmission due to the potential for worsening muscle weakness. It should be used very cautiously, if at all, in patients with heart block, as it can exacerbate conduction defects. Magnesium is contraindicated in patients with severe renal impairment (CrCl <30 ml/min) due to the risk of hypermagnesemia.
Drug Interactions
Magnesium can decrease the absorption of oral bisphosphonates, fluoroquinolone and tetracycline antibiotics, and levothyroxine – these drugs should be taken at least 2 hours before or 4-6 hours after magnesium salts. It may enhance the neuromuscular blocking effects of nondepolarizing agents such as rocuronium and cisatracurium. Potent diuretics can increase urinary magnesium losses. Prolonged use of proton pump inhibitors may lead to hypomagnesemia.
Conclusion
Magnesium sulfate is an important medication with a variety of clinical applications, supported by its unique pharmacological properties. Understanding its mechanisms of action, pharmacokinetics, indications, and potential adverse effects is essential for its safe and effective use. As with all drugs, the risks and benefits must be carefully weighed in each patient scenario.









