Pharmacology of Antiviral Drugs
Comprehensive Pharmacology of Antiviral Drugs Compiled May 01 2025 Introduction Antiviral pharmacology has advanced from the single-agent era of idoxuridine to a modern arsenal including polymerase terminators, protease blockers, monoclonal…
Pharmacotherapy of Type 1 Diabetes Mellitus
Introduction Type 1 diabetes mellitus (T1DM) is a complex autoimmune disorder requiring comprehensive pharmacological management throughout the patient's lifetime. Since the discovery of insulin over a century ago, numerous advancements…
Broad spectrum antibiotics – Tetracyclines and Chloramphenicol
Introduction Broad-spectrum antibiotics stand at the forefront of infectious disease management, enabling healthcare professionals to effectively target a wide variety of bacterial pathogens without waiting for definitive culture results. Within…
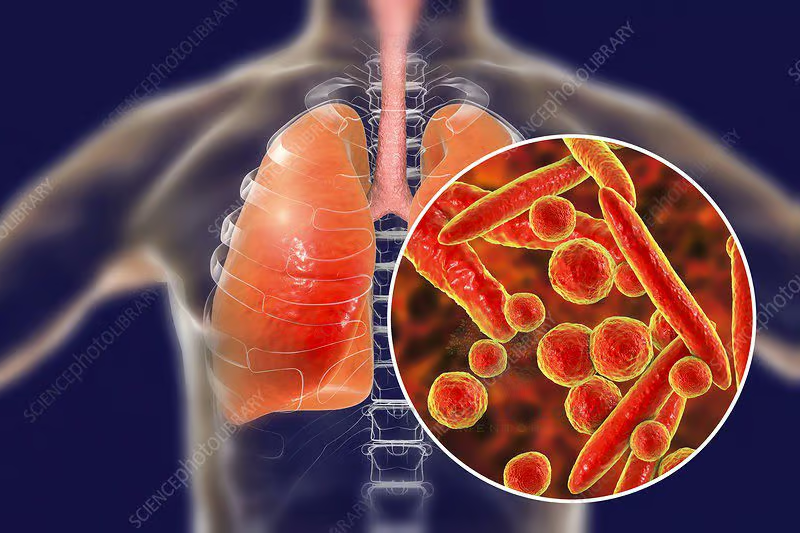
A review on drug resistant mycoplasma pneumonia
Introduction Mycoplasma pneumoniae is a unique bacterial pathogen that causes a spectrum of respiratory infections, ranging from mild tracheobronchitis to severe pneumonia . Unlike many typical bacteria, it lacks a…
Pharmacotherapy of erectile dysfunction
Introduction Erectile dysfunction (ED), defined as the consistent or recurrent inability to attain or maintain an erection sufficient for satisfactory sexual performance, affects millions of men worldwide. Though once considered…
Pharmacotherapy of migraine
Introduction Migraine is a debilitating primary headache disorder characterized by episodic attacks of throbbing or pulsating head pain, often accompanied by photophobia, phonophobia, nausea, and in some cases, aura phenomena.…
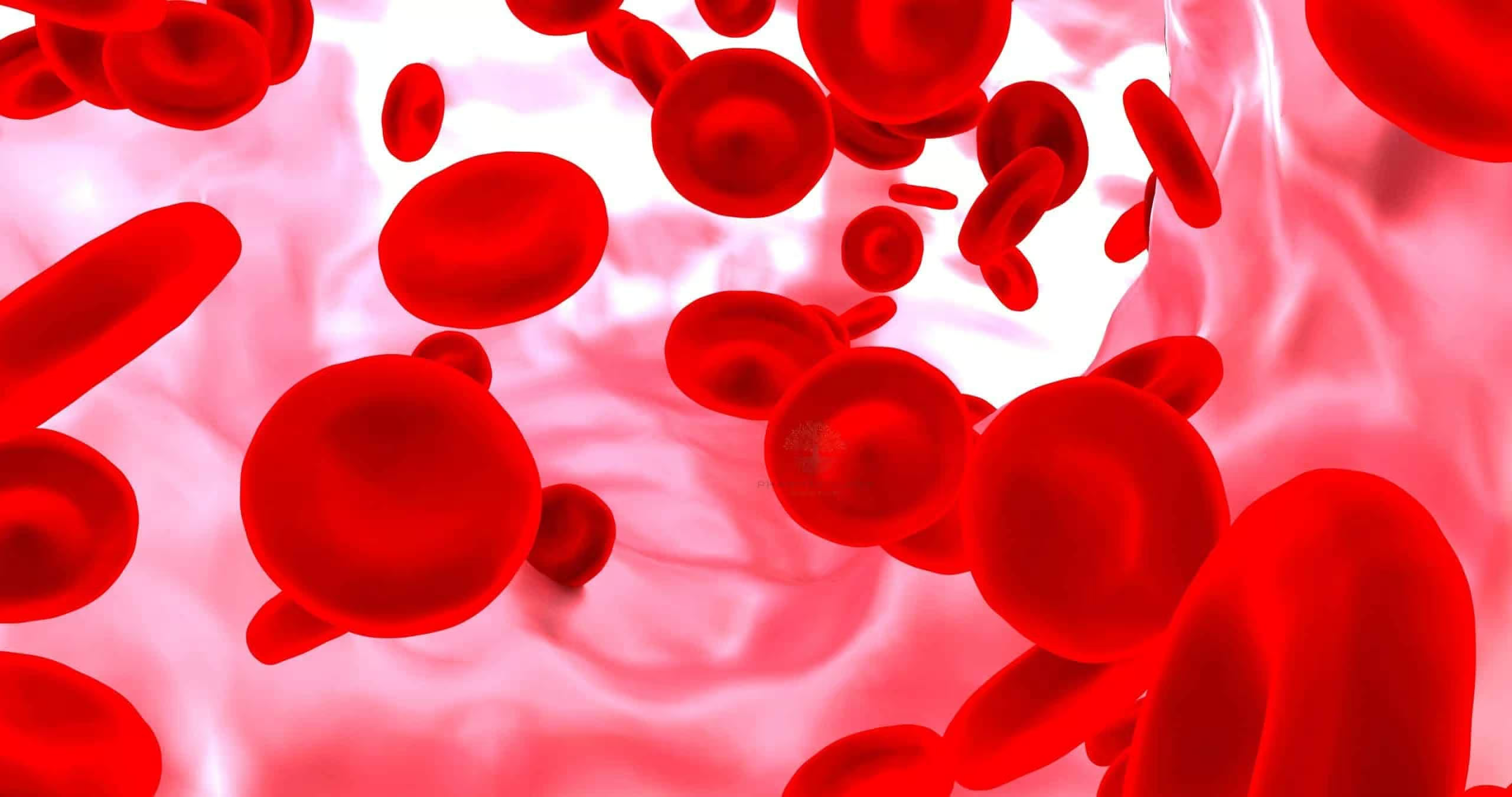
Pharmacology of Fibrinolytics
Introduction Fibrinolytics—also known as thrombolytics—are a specialized class of pharmacological agents that dissolve blood clots (thrombi) by catalyzing the conversion of plasminogen to plasmin, the main fibrinolytic enzyme. These drugs…
Pharmacology of anticoagulants
Introduction Anticoagulants constitute an essential class of drugs used to inhibit blood coagulation, ultimately preventing or treating thromboembolic disorders such as deep vein thrombosis (DVT), pulmonary embolism (PE), and stroke in…
Pharmacology of Antiplatelet Drugs
Introduction Platelets play a pivotal role in hemostasis, forming plugs that stem bleeding after vascular injury. However, when platelet activity becomes dysregulated or excessive, it can precipitate arterial thrombosis, leading…
What is Pharmacology? An introduction
1 · Definition & Conceptual Overview Pharmacology is the scientific discipline that investigates how chemical agents (drugs) interact with living systems to modify physiological or biochemical functions. At its core,…