Introduction
Selective Serotonin Reuptake Inhibitors (SSRIs) revolutionized the treatment of depression and related affective disorders in the late 20th century. Since their introduction, SSRIs have become the first-line pharmacological treatment for mild, moderate, and even severe depressive episodes. Beyond depression, these drugs find a broad spectrum of applications, including anxiety disorders, obsessive-compulsive disorder (OCD), post-traumatic stress disorder (PTSD), eating disorders, and premenstrual dysphoric disorder (PMDD). SSRIs owe their popularity to relatively favorable tolerability, lower lethality in overdose, and fewer side effects compared to older antidepressants like tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) (Goodman & Gilman, 2018; Katzung, 2020).
Despite their widespread use, SSRIs remain complex agents whose pharmacodynamics, pharmacokinetics, safety profiles, and clinical toxicity demand ongoing refinement of clinical practice. A thorough comprehension of their mechanisms—particularly their influence on the serotonin transporter (SERT)—is essential for providing optimal therapeutic outcomes. This article provides a comprehensive look at SSRI pharmacotherapy, detailing their discovery, mechanism of action, pharmacokinetic properties, clinical uses, side effects, and newer scientific frontiers. By integrating insights from major pharmacology references and the latest guidelines, we offer an in-depth resource for both clinicians and students aiming at a nuanced grasp of SSRIs.
Discovery and Evolution of SSRIs
Conventional antidepressants, like TCAs, were effective yet fraught with significant anticholinergic and cardiotoxic side effects. The understanding that serotonin (5-HT) deficiency contributed substantially to depressive pathology encouraged researchers to develop drugs selectively targeting the 5-HT system. Fluoxetine, introduced in the late 1980s, marked the dawn of SSRIs, offering safer overdose profiles, less sedation, and fewer cardiovascular issues (Rang & Dale, 2019). Over the past three decades, more SSRIs emerged, each wielding subtle pharmacodynamic differences. Despite these variations, the central principle remains the same: selectively enhancing serotonergic neurotransmission by inhibiting the reuptake of serotonin at presynaptic neurons.
First-generation SSRIs—starting with fluoxetine—ushered in an era of improved tolerability. Successive developments—sertraline, paroxetine, citalopram, escitalopram, and fluvoxamine—have honed the selectivity for SERT, reducing off-target binding. This refinement fosters a better side-effect profile relative to older antidepressants (Goodman & Gilman, 2018). Retaining robust efficacy for depression, SSRIs also gained regulatory approvals for various anxiety and stress-related disorders, expanding their utility. Understanding nuances in receptor binding, enzyme inhibition, and half-lives guides precise drug choice for individual patients.
Mechanism of Action
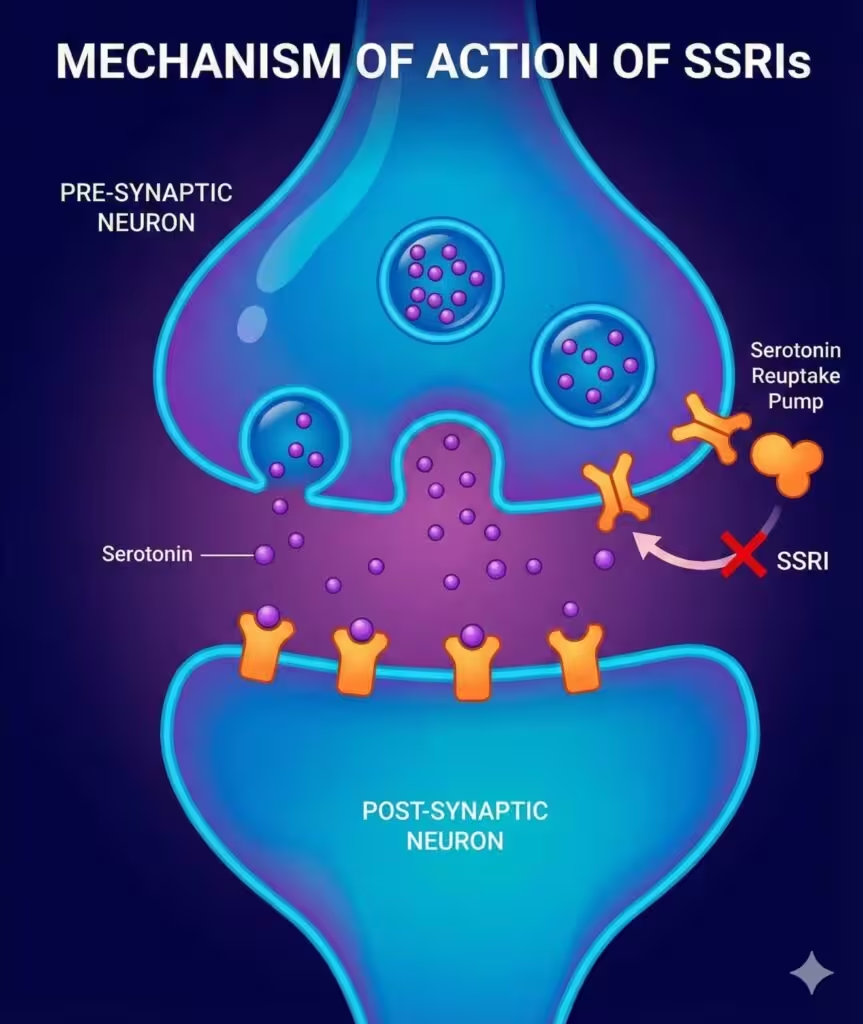
Serotonin Reuptake Inhibition
SSRIs exert their primary effect by blocking the serotonin transporter (SERT) on presynaptic neurons, preventing reabsorption of 5-HT into the presynaptic terminal. This mechanism prolongs the synaptic availability of serotonin, reinforcing postsynaptic receptor activation. Over time, adaptive downstream changes (e.g., receptor sensitivity alterations, neurotrophic factor expression changes) contribute to the antidepressant and anxiolytic effects (Katzung, 2020).
The increased serotonin concentration amplifies signaling through 5-HT1A and, to some extent, 5-HT2 receptor subtypes in the brain’s mood-regulation areas. SSRIs do not directly affect the reuptake of norepinephrine (NE) or dopamine (DA) to a substantial degree, distinguishing them pharmacologically from SNRIs or bupropion. Despite their “selective” label, SSRIs differ subtly in off-target receptor interactions (e.g., histamine or muscarinic blockade), explaining certain side-effect differences across the class.
Downstream Neurochemical Adaptations
The immediate boost in synaptic 5-HT does not fully explain the temporal lag—often several weeks—before symptom relief emerges. Chronic SSRI administration leads to complex downstream events:
• Desensitization of presynaptic autoreceptors and certain postsynaptic receptors, modulating further serotonin release and receptor responsiveness.
• Gene transcription changes in neuronal plasticity markers (e.g., brain-derived neurotrophic factor, BDNF), promoting synaptic remodeling and resilience in key mood circuit regions (Goodman & Gilman, 2018).
• Interplay with other neurotransmitters—like gamma-aminobutyric acid (GABA) and glutamate—shapes a broader homeostatic realignment conducive to improved mood and anxiety control.
Commonly Prescribed SSRIs
Fluoxetine
Fluoxetine (Prozac) was the prototype SSRI, known for its relatively long half-life (~2–3 days) and active metabolite (norfluoxetine) with a half-life of up to two weeks. The long elimination phase can reduce withdrawal symptoms but complicates polypharmacy if a patient switches antidepressants (Rang & Dale, 2019). Fluoxetine has mildly stimulating properties, making it potentially beneficial for patients with low energy but possibly exacerbating anxiety or insomnia.
Sertraline
Sertraline (Zoloft) demonstrates potent SERT inhibition, moderate dopamine transporter (DAT) inhibition, and minimal drug interactions. It has a half-life of 24–26 hours, typically well-tolerated, though it may potentiate GI side effects at higher doses. Sertraline is often favored for comorbid anxiety, OCD, and PTSD (Katzung, 2020).
Paroxetine
Paroxetine (Paxil) is known for its comparatively anticholinergic activity, which can cause sedation, weight gain, and constipation. It strongly inhibits CYP2D6, raising potential for drug interactions. Paroxetine also shows notable discontinuation syndrome if abruptly stopped, owing to its shorter half-life and absence of active metabolites. Clinically, it sees use in generalized anxiety disorder (GAD), panic disorder, and major depression (Goodman & Gilman, 2018).
Fluvoxamine
Fluvoxamine (Luvox) is especially indicated for OCD, though it can treat depression and anxiety as well. It can inhibit CYP1A2 and CYP2C19, warranting attention to interactions with theophylline, warfarin, and other susceptible drugs. Its half-life is ~15 hours, making it typically dosed once or twice daily (Rang & Dale, 2019).
Citalopram and Escitalopram
Citalopram (Celexa) and its S-enantiomer escitalopram (Lexapro) enjoy popularity due to balanced efficacy, fewer CYP-related interactions, and a well-tolerated side-effect profile. Escitalopram is often described as among the most selective SSRIs with a relatively favorable cardiovascular profile, though citalopram at higher doses may prolong the QT interval, requiring ECG monitoring for those with risk factors (Katzung, 2020).
Pharmacokinetics
Absorption and Distribution
SSRIs are well absorbed from the GI tract, achieving peak plasma levels in 4–8 hours, though absorption can vary by molecule’s lipid solubility. Generally, SSRIs exhibit high volume of distribution, given their lipophilic structure, and they can accumulate in tissues (Goodman & Gilman, 2018).
Metabolism
Hepatic CYP450 isoenzymes (like CYP2D6, CYP3A4, CYP2C9, CYP2C19) predominantly metabolize SSRIs. Fluoxetine, paroxetine, and fluvoxamine can inhibit specific CYP enzymes, potentially raising serum concentrations of co-prescribed drugs (e.g., certain antiarrhythmics, beta-blockers, antipsychotics). In contrast, sertraline, citalopram, and escitalopram exhibit milder inhibitory effects, posing fewer interaction concerns (Rang & Dale, 2019).
Elimination
Plasma half-lives range from ~1 day (paroxetine, sertraline) to up to 2–3 days (fluoxetine) or longer for active metabolites. This variability affects dose adjustment, possible accumulation, drug washout, and the intensity of discontinuation symptoms. Typically, SSRIs are administered once daily, taking advantage of their relatively long half-lives and consistent receptor occupancy (Katzung, 2020).
Clinical Indications
Although major depressive disorder (MDD) remains the principal use, SSRIs address a broad range of psychiatric conditions:
- Depression: Single episodes or recurrent MDD; recommended first-line due to tolerability and effectiveness.
- Anxiety Disorders: SSRIs effectively manage GAD, social anxiety, panic disorder, PTSD, and OCD. They often require slightly higher doses and longer titration for OCD (Goodman & Gilman, 2018).
- Premenstrual Dysphoric Disorder (PMDD): SSRIs like fluoxetine or sertraline can alleviate emotional and physical PMDD symptoms.
- Eating Disorders: Fluoxetine is approved for bulimia nervosa; SSRIs may also help coexisting depression in anorexia or binge eating, though efficacy is less consistent.
- Chronic Pain Syndromes: Some SSRIs help neuropathic pain, albeit less robustly than SNRIs. Escitalopram or sertraline might be considered if depression coexists with mild pain (Katzung, 2020).
- Other Off-Label Uses: SSRIs occasionally address pathological gambling, certain impulse control disorders, and comorbid depression in chronic medical conditions.
Regardless of indication, a thorough baseline assessment is vital to choose doses, anticipate side effects, and manage potential drug interactions.
Dose, Administration, and Treatment Duration
Initiation and Titration
Therapeutic doses vary among SSRIs. For instance, fluoxetine often starts at 20 mg/day, sertraline at 50 mg/day, paroxetine at 20 mg/day, citalopram at 20 mg/day, and escitalopram at 10 mg/day. Doses can be incrementally increased every 2–4 weeks if clinical response remains insufficient (Rang & Dale, 2019). Lower initial doses help minimize side effects, especially in anxiety disorders, where SSRIs can transiently heighten anxiety upon initiation.
Time to Therapeutic Response
Most patients experience some improvement in energy, sleep, or appetite within 1–2 weeks. However, 4–6 weeks or longer may pass before a robust antidepressant effect emerges. For OCD, the onset can take even longer—up to 8–12 weeks. Tailoring expectations and ensuring adherence is crucial, as premature discontinuation stifles potential benefits (Katzung, 2020).
Maintenance and Relapse Prevention
Guidelines generally advise continuing SSRIs for at least 6–12 months after achieving remission from a first major depressive episode. Longer maintenance (1–2 years or indefinite) is recommended for recurrent depression or chronic anxiety conditions to reduce relapse risk. Regular re-evaluation helps weigh ongoing benefits against medication burdens (Goodman & Gilman, 2018).
Adverse Effects
Gastrointestinal Upset
Nausea, diarrhea, and dyspepsia commonly occur, particularly early in treatment. These GI effects often abate within 1–2 weeks but can persist in some patients. Dividing doses or taking medication with food may help mitigate severity (Rang & Dale, 2019).
Sexual Dysfunction
One of the most frequent reasons for non-adherence is sexual side effects, such as decreased libido, anorgasmia, or erectile dysfunction. Paroxetine often poses the highest risk, while bupropion (an NDRI) or mirtazapine (an alpha-2 antagonist) sometimes substitutes for SSRIs when sexual dysfunction is intolerable. Strategies like dose reduction, “drug holidays,” or adjunctive agents (e.g., sildenafil) occasionally prove beneficial (Katzung, 2020).
Weight Changes
Weight fluctuations can vary: paroxetine is somewhat associated with weight gain, while fluoxetine or sertraline might be weight-neutral or cause slight weight loss initially. Chronic use for months to years can still result in modest net weight gain (Goodman & Gilman, 2018).
Central Nervous System Effects
Some patients experience insomnia or vivid dreams, especially with more activating SSRIs like fluoxetine or sertraline. Conversely, paroxetine might cause sedation. SSRIs can sometimes heighten anxiety or restlessness, particularly in the early weeks (Rang & Dale, 2019).
Suicidality Risk in Younger Patients
An FDA black box warning cites increased suicidal ideation in children, adolescents, and young adults during initial treatment. Close monitoring, especially in the first few weeks, is recommended. Long-term data, however, suggest that effectively treated depression overall reduces suicide risk (Katzung, 2020).
Serotonin Syndrome
Excessive serotonergic activity, possibly from combining SSRIs with MAO inhibitors, SNRIs, triptans, or other serotonergic drugs, can precipitate serotonin syndrome. Symptoms include agitation, confusion, myoclonus, hyperreflexia, sweating, tremor, and in severe cases, hyperthermia, and muscle rigidity. Prompt recognition and discontinuation of implicated agents, plus supportive care, are paramount (Goodman & Gilman, 2018).
Bleeding Diathesis
SSRIs inhibit platelet serotonin uptake, potentially impairing platelet aggregation. Concomitant use with NSAIDs or anticoagulants slightly elevates the risk of gastrointestinal bleeding. Patients at high bleed risk should be monitored or switched to an alternative antidepressant or provided gastroprotective measures (Rang & Dale, 2019).
Hyponatremia / SIADH
By unclear mechanisms, SSRIs can induce syndrome of inappropriate antidiuretic hormone secretion (SIADH), leading to hyponatremia—particularly in older adults or those with other predisposing factors. Checking electrolytes if confusion or other suspicious symptoms arise is prudent (Katzung, 2020).
Drug Interactions
- Monoamine Oxidase Inhibitors (MAOIs): Concurrent use is contraindicated, requiring a washout period (2 weeks for most SSRIs; 5 weeks for fluoxetine) to avert serotonin syndrome.
- Triptans / Other Serotonergic Agents: Heightened risk of serotonin syndrome. Caution with tramadol, linezolid, and St. John’s wort.
- Warfarin / Other Anticoagulants: Elevated risk of bleeding, especially with highly protein-bound SSRIs or those that affect platelet function.
- CYP Enzyme Inhibitions: Paroxetine, fluoxetine, and fluvoxamine can drastically raise levels of certain drugs metabolized by CYP2D6 or CYP3A4 (Goodman & Gilman, 2018). Checking concomitant medications is vital for safe prescribing.
Discontinuation Syndrome
Abrupt cessation of SSRIs with shorter half-lives (paroxetine, sertraline) can precipitate discontinuation symptoms—dizziness, irritability, sensory disturbances (electric shock-like “brain zaps”), mood swings, and flu-like symptoms. Tapering over 2–4 weeks mitigates these effects (Rang & Dale, 2019). Fluoxetine’s prolonged half-life typically averts severe withdrawal, although some mild discontinuation issues can still arise if stopping high doses.
Overdose and Toxicity
SSRI overdoses generally produce fewer cardiac complications versus TCAs (e.g., no significant QRS prolongation). Nonetheless, large overdoses may induce seizures, serotonin syndrome, or severe CNS depression. Supportive measures—airway management, activated charcoal if timely, and monitoring for arrhythmias—are the mainstays of acute management (Katzung, 2020). While SSRIs alone rarely prove fatal in overdose, co-ingestion of other drugs (especially sedatives, opioids, or alcohol) raises morbidity and mortality.
Special Populations
Pediatric Patients
SSRIs are commonly used for pediatric depression or OCD, with careful monitoring for suicidal ideation. Fluoxetine is FDA-approved for ages 8 and older in MDD, and for OCD in ages 7 and older. Sertraline is approved for OCD in children 6 and older, while escitalopram can be used for adolescents with depression. Dosing typically starts low, with vigilant follow-up (Goodman & Gilman, 2018).
Geriatric Patients
Elderly individuals can benefit from SSRIs for depression or anxiety, but they may be more prone to hyponatremia, drug-drug interactions, and sedation/falls. Citalopram and escitalopram are often favored, given moderate half-lives and lower potential for interactions. Checking for orthostatic hypotension, electrolytes, and sedation is advisable (Rang & Dale, 2019).
Pregnancy and Lactation
Untreated maternal depression poses serious risks; SSRIs are comparatively safer vs. older antidepressants, though concerns exist about potential pulmonary hypertension in newborns or mild withdrawal if used late in pregnancy. Sertraline and fluoxetine are frequently used, but paroxetine is generally downgraded due to possible fetal cardiac risks. Balancing the mother’s mental health with fetal safety is essential (Katzung, 2020).
Comorbid Medical Conditions
Patients with significant medical illnesses—particularly hepatic impairment—may require dose adjustments. In hepatic dysfunction, SSRIs can accumulate. Cardiovascular comorbidities largely do not contraindicate SSRIs, aside from monitoring citalopram’s QT-prolonging effect. SSRIs’ minimal sedation and orthostatic effect are beneficial for unstable cardiovascular patients (Goodman & Gilman, 2018).
Comparative Profiles and Tailoring Therapy
Efficacy Across the Class
Head-to-head trials often reveal similar efficacy among SSRIs for depression. Hence, drug choice frequently hinges on tolerability, drug interaction profile, patient preference, and specific symptom profiles. For instance:
• Sertraline or escitalopram are first-line for depression plus anxiety.
• Fluoxetine might be beneficial for patients with low energy or mild sedation needs.
• Paroxetine may help intense anxiety or insomnia but has higher sedation and withdrawal issues (Rang & Dale, 2019).
Considerations for Specific Symptoms
- Fatigue, low energy: A more activating SSRI (fluoxetine or sertraline) may help.
- Insomnia: A more sedating SSRI (paroxetine) or evening dosing may be beneficial.
- Sexual Dysfunction: If intolerable, switching to bupropion or mirtazapine, or augmenting with PDE5 inhibitors, can help.
- Frequent GI side effects: Start at lower doses, switch to an alternative SSRI or to an SNRI if persistent.
Research on Augmentation and Combination Strategies
Augmentation with Other Agents
For partial or non-responders to SSRIs, augmentation with second agents can enhance efficacy:
- Atypical antipsychotics (e.g., aripiprazole, quetipine) beneficial for treatment-resistant depression.
- Lithium or thyroid hormone (T3) in some long-standing augmentation protocols.
- Buspirone or low-dose mirtazapine for persistent anxiety or to mitigate SSRI-induced sexual dysfunction (Katzung, 2020).
Combination with Psychotherapy
Cognitive behavioral therapy (CBT) plus SSRIs can yield superior outcomes in depression, anxiety, and OCD. Psychological interventions address maladaptive cognitions and coping deficits, complementing the neurochemical normalization SSRIs provide (Goodman & Gilman, 2018).
Novel Perspectives and Future Directions
Precision Psychiatry and Pharmacogenomics
Genetic polymorphisms in CYP2D6, CYP2C19, or serotonin receptors/transporters might influence SSRI metabolism and response. Pharmacogenetic testing is gaining ground, though large-scale evidence for routine testing remains tentative. Emerging technologies promise to refine personalized medication selection, dosage, and side-effect management (Rang & Dale, 2019).
Rapid-Acting Antidepressants
The success of ketamine and related N-methyl-D-aspartate (NMDA) receptor modulators for treatment-resistant depression highlights the limitations of classic SSRIs’ delayed onset. Ongoing research attempts to combine or modify SSRIs with adjunct processes—like neurosteroids, anti-inflammatory or neuropeptide agents—to accelerate the antidepressant effect (Katzung, 2020).
Biomarkers and Endophenotypes
To date, no robust biomarkers predict SSRI response, though functional neuroimaging measures or peripheral factors (e.g., BDNF or inflammatory cytokines) may eventually guide therapy. Future breakthroughs could identify subgroups more responsive to SSRIs or better served by alternative classes (Goodman & Gilman, 2018).
Clinical Pearls and Practical Recommendations
- Start Low, Go Slow: Initiate SSRIs at modest doses, especially in anxious or medically frail individuals. Titrate gently to mitigate side effects.
- Monitor Response: Use standardized scales (e.g., PHQ-9, HAM-D) to track improvement over 4–8 weeks.
- Assess Side Effects Continuously: Sexual dysfunction, insomnia, GI upset are leading reasons for dropout. Elicit these concerns proactively.
- Avoid Abrupt Discontinuation: Taper SSRIs—particularly paroxetine—to circumvent severe discontinuation symptoms.
- Check for Interactions: Evaluate concurrent medication regimens for overlapping serotonergic or CYP-metabolized agents.
- Long-Term Strategy: For recurrent depression or anxiety, a maintenance plan (often 1 year or longer) fosters sustained remission.
- Lifestyle and Therapy: Encourage exercise, balanced diet, social support, and possibly psychotherapy to augment medication efficacy (Rang & Dale, 2019; Katzung, 2020).
Conclusion
SSRIs remain foundational in modern psychiatry for their efficacy in treating depression, anxiety disorders, OCD, PMDD, and other conditions. Their relative safety compared with older antidepressants—particularly regarding systemic toxicities and overdose risk—has made them the first-line choice in most treatment guidelines. Understanding the mechanistic nuance (selective inhibition of serotonin reuptake), pharmacokinetic profiles (hepatic metabolism, half-life variations), and side-effect spectrum (sexual dysfunction, GI effects, potential for weight change, risk of serotonin syndrome) informs rational prescribing.
With an expanding array of SSRIs on the market, clinicians can tailor drug selection and dosing to each patient’s symptom profile, comorbid conditions, and vulnerability to adverse effects. Nonetheless, challenges remain—sexual dysfunction frequently interrupts adherence, while some patients see incomplete remission or relapse. Emerging research into augmentation strategies, pharmacogenetics, and novel rapid-onset mechanisms aims to surmount these hurdles (Goodman & Gilman, 2018).
Long-term studies underscore SSRIs’ utility in preventing recurrence of depressive and anxiety disorders, reinforcing the importance of sustained therapy and supportive measures beyond acute symptomatic relief. By staying abreast of drug interactions, the potential for discontinuation syndrome, and patient-specific risk factors, clinicians can optimize SSRI therapy and significantly enhance patient well-being and functional recovery (Katzung, 2020; Rang & Dale, 2019).
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- Katzung BG, Basic & Clinical Pharmacology, 14th Edition.
- Rang HP, Dale MM, Rang & Dale’s Pharmacology, 8th Edition.
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.

