I. Introduction and Definition
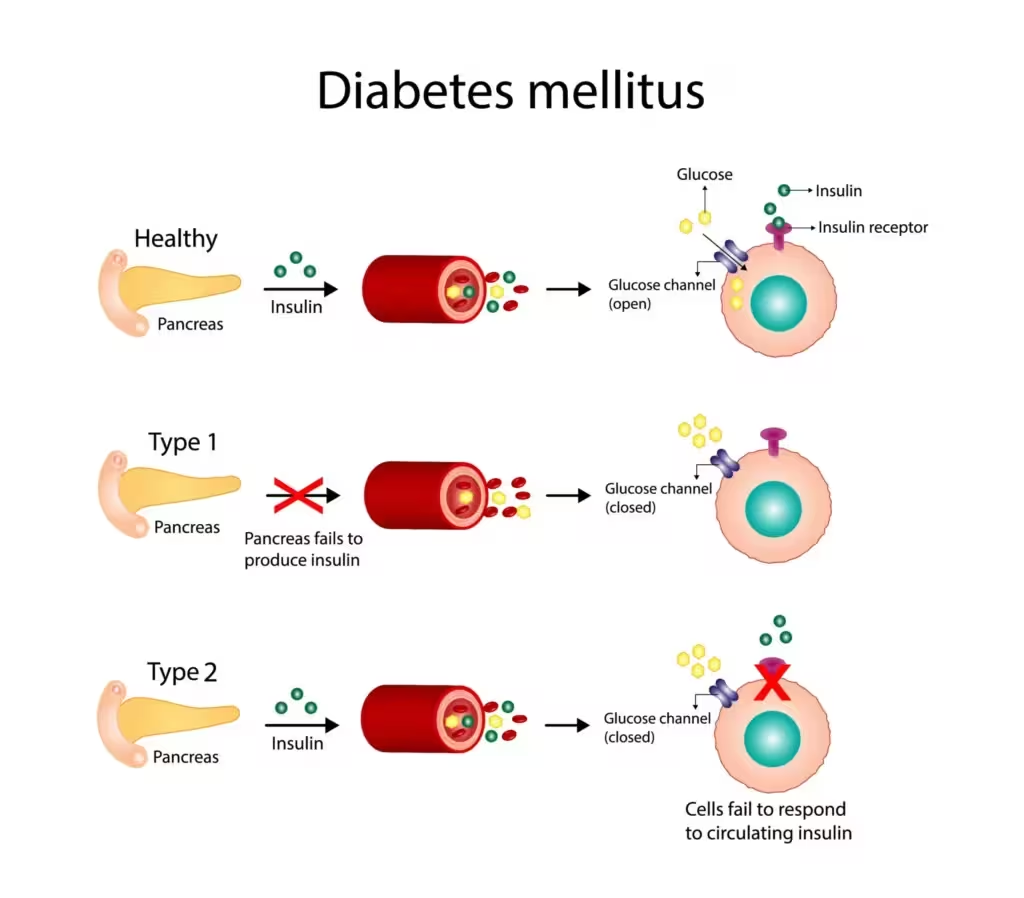
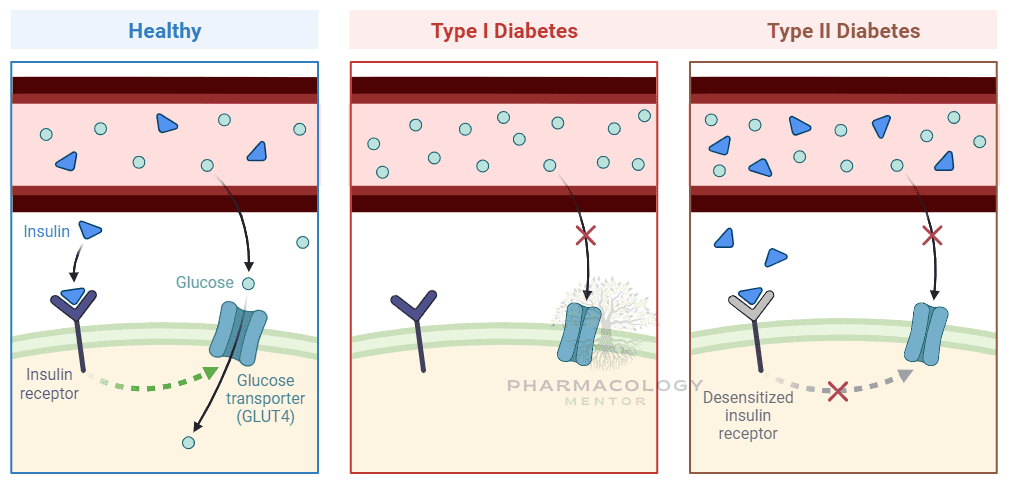
Diabetes mellitus defines a group of inherited and acquired metabolic disorders marked by hyperglycemia resulting from absolute (Type 1) or relative (Type 2) deficiencies in insulin secretion, insulin action, or both. Chronic hyperglycemia leads to multisystem complications impacting eyes, kidneys, nerves, cardiovascular and immune systems.
II. Types and Epidemiology
A. Major Types
- Type 1 diabetes mellitus (T1DM): Autoimmune destruction of pancreatic β-cells causing absolute insulin deficiency. Usually manifests in childhood or adolescence, but can present at any age.
- Type 2 diabetes mellitus (T2DM): Ranges from predominantly insulin resistance with relative insulin deficiency to an insulin secretory defect with insulin resistance. Typically adult-onset, but now seen in youths.
- Other types: MODY (maturity-onset diabetes of the young), secondary diabetes (pancreatic disease, drugs, endocrinopathies), and gestational diabetes mellitus (GDM: glucose intolerance during pregnancy).
B. Epidemiology
- Diabetes affects >425 million people globally. Type 2 is >90% of cases.
- Rapidly increasing in developing nations linked to obesity, sedentary lifestyle, and aging populations.
III. Etiology and Pathogenesis
A. Type 1 DM
- Genetics: HLA associations (DR3, DR4)
- Autoimmunity: Anti-islet cell and anti-insulin autoantibodies.
- Pathogenesis: Triggered by environmental factors (viral infection, toxins) in genetically susceptible individuals; immune-mediated destruction leads to absence of insulin secretion.
B. Type 2 DM
- Genetics: Polygenic, strong familial link.
- Obesity and sedentary lifestyle: Central obesity is key.
- Insulin resistance: Skeletal muscle, liver, adipose.
- β-cell dysfunction: Defective insulin synthesis/secretion fails to compensate for resistance.
C. Other causes
- Genetic defects of β-cell function (MODY)
- Genetic defects of insulin action (leprechaunism, Rabson–Mendenhall)
- Pancreatic disease (pancreatitis, cystic fibrosis)
- Endocrinopathies (Cushing, acromegaly, pheochromocytoma)
- Drug-induced (glucocorticoids, thiazides, atypical antipsychotics).
IV. Clinical Presentation—Symptoms and Diagnosis
A. Classic Symptoms
- Polyuria, polydipsia, polyphagia
- Unintentional weight loss (T1DM)
- Fatigue, blurry vision, recurrent infections
- In T2DM: insidious onset, sometimes discovered incidentally
B. Complications at diagnosis
- Diabetic ketoacidosis (DKA)—often first manifestation in T1DM
- Hyperosmolar hyperglycemic state (HHS)—severe hyperglycemia without ketones, fluid depletion (T2DM)
C. Diagnostic criteria (ADA/WHO)
- Fasting plasma glucose (FPG) ≥126 mg/dL (7.0 mmol/L)
- 2-h plasma glucose ≥200 mg/dL (11.1 mmol/L) during OGTT
- HbA1c ≥6.5%
- Random plasma glucose ≥200 mg/dL with symptoms
—criteria should be confirmed on repeat testing unless unequivocal.
V. Pathophysiology: Consequences of Chronic Hyperglycemia
- Acute: Polyuria/polydipsia, ketoacidosis, HHS.
- Chronic:
VI. Non-pharmacological Management
- Lifestyle modification: Nutritional therapy (carbohydrate control, fat/salt restriction), regular exercise, weight reduction, smoking cessation.
VII. Pharmacological Treatment
A. Insulin
Indications: All T1DM, many T2DM after failure of oral agents, acute illness, pregnancy.
- Types: Rapid–, short– (regular), intermediate– (NPH), long–acting (glargine, detemir, degludec), premixed.
- Regimens: Basal–bolus, premixed, continuous subcutaneous infusion (pumps).
- Adverse effects: Hypoglycemia (major risk), weight gain, injection-site reactions, lipodystrophy.
B. Oral and Non-insulin Injectables (T2DM)
1. Biguanides
- Metformin. First-line agent for overweight T2DM.
- Mechanism: Inhibits hepatic gluconeogenesis and insulin resistance.
- Benefits: No hypoglycemia, probable CV benefit, weight neutral/loss.
- Adverse: GI upset, lactic acidosis (avoid in eGFR <30 ml/min).
2. Sulfonylureas
- Glibenclamide, glipizide, gliclazide, glimepiride.
- Mechanism: Stimulate insulin release from β-cells (KATP blocker).
- Risk: Hypoglycemia, weight gain.
3. Meglitinides (glinides)
- Repaglinide, nateglinide; shorter-acting, pre-meal dosing.
4. Thiazolidinediones (TZDs)
- Pioglitazone, rosiglitazone.
- Mechanism: PPAR-γ agonists, enhance insulin sensitivity.
- Risks: Weight gain, edema, HF risk, fractures.
5. DPP-4 Inhibitors (gliptins)
- Sitagliptin, linagliptin, saxagliptin.
- Mechanism: Inhibit incretin breakdown, increasing GLP-1/GIP.
- Safe: Neutral for weight and low hypoglycemia risk.
6. GLP-1 Receptor Agonists (injectable)
- Exenatide, liraglutide, dulaglutide.
- Mechanism: Incretin mimetics—increase insulin, decrease glucagon, slow gastric emptying.
- Benefits: Weight loss, CV protection (some), low hypoglycemia.
- Adverse: Nausea, injection reactions.
7. SGLT2 Inhibitors
- Dapagliflozin, empagliflozin, canagliflozin.
- Mechanism: Block renal glucose resorption, glucuresis.
- Benefits: Weight loss, mild BP lowering, notable CV/renal protection.
- Risks: Genital infections, euglycemic DKA.
8. Alpha-glucosidase inhibitors
- Acarbose, miglitol.
- Mechanism: Delay carbohydrate absorption; useful for postprandial hyperglycemia.
- Adverse: Flatulence, diarrhea.
9. Others (rare): Pramlintide (amylin analogue), colesevelam, bromocriptine.
VIII. Special Approaches and Treatment Nuances
- Initial agent: Metformin unless contraindicated.
- Dual/triple therapy: As per need, patient profile, and comorbidity.
- Early insulinization: When marked hyperglycemia, ketosis, or advanced catabolism present.
- Cardiometabolic protection: Use GLP-1RA or SGLT2i with proven CV benefit where indicated (CV disease, CKD, HF).
- Elderly/frail: Avoid hypoglycemic agents, individualize targets.
IX. Monitoring and Follow-Up
- Glycemic monitoring: Self-monitoring of blood glucose (SMBG), HbA1c every 3-6 months.
- Complications surveillance: Annual microalbuminuria, eGFR, eye examination (retinal photography), foot checks.
- Targets: FPG 80–130 mg/dL, postprandial <180, individualized HbA1c (usually <7% for most, less stringent for older/comorbid).
X. Management of Complications
A. Acute
- DKA: Emergency. Fluids, IV insulin, K+ replacement, treat precipitant.
- HHS: Similar but more insidious, more severe dehydration, less ketosis.
- Hypoglycemia: Rapid glucose (oral, IV dextrose, glucagon if unconscious).
B. Chronic—Prevention
- Retinopathy: Regular screening, glycemic and BP control.
- Nephropathy: BP control (ACE/ARB), glycemic control.
- Neuropathy: Glycemic control, pain control as needed.
- Macrovascular: Aggressive CV risk factor management (BP, lipids, antiplatelets).
XI. Diabetes in Special Populations
- Pregnancy: Insulin is gold standard; oral agents generally avoided.
- Children: T1DM common; use basal–bolus strategies.
- CKD: Dose adjust most oral agents; avoid metformin if GFR<30.
- Elderly: Avoid tight target, sulfonylureas if high hypoglycemia risk.
XII. Patient Education and Self-Management
- Nutrition and carbohydrate counting (especially in T1DM).
- Insulin administration and hypoglycemia recognition.
- Infection prevention, foot care, regular monitoring.
- Sick-day rules.
XIII. Future Directions
- Closed-loop insulin delivery (“artificial pancreas”)
- Beta-cell replacement and regenerative therapies
- Oral GLP-1 agonists, new co-formulations, gene editing prospects
XIV. Tables
Table A: Drug Classes for T2DM
| Class | Example Drugs | Mechanism | Main Adverse Effects | Comments |
|---|---|---|---|---|
| Biguanides | Metformin | ↓ Gluconeogenesis, ↑ Insulin sens. | GI, B12 def, lactic acidosis (rare) | First-line; stop in severe CKD/IV contrast |
| Sulfonylureas | Glipizide, Glyburide | ↑ Insulin secretion | Hypoglycemia, weight gain | Avoid in elderly with hypoglycemia risk |
| SGLT2 inhibitors | Dapagliflozin | ↑ Renal glucose excretion | UTI, mycotic inf., euglycemic DKA | CV/renal benefits, weight loss |
| DPP-4 inhibitors | Sitagliptin | ↑ Endogenous incretin activity | Nasopharyngitis, rare pancreatitis | CV neutral, safe in CKD (some) |
| GLP-1 RA | Liraglutide | ↑ Insulin, ↓ Glucagon, Gastric delay | GI, wt loss, pancreatitis (rare) | CV benefit, injectables |
| TZDs | Pioglitazone | ↑ Insulin sensitivity via PPAR-γ | Edema, HF, weight gain, fractures | Avoid in HF, bladder CA suspicion |
XV. Key Learning Points
- Diabetes is a multifactorial chronic disease—manage BOTH glycemic and holistic cardiometabolic risk.
- Pharmacological therapy individualized for efficacy, risk, comorbidity, age, patient preference.
- Lifestyle interventions and self-management are always foundational.
- Frequent monitoring and complication screening is key for morbidity and mortality reduction.
- Newer agents provide not only glucose control but CV/renal protection—should be prioritized in high-risk patients.
XVI. References
- Brunton LL, Hilal-Dandan R, Knollmann BC, eds. Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 13th ed. New York: McGraw-Hill; 2017. Diabetes mellitus and management.
- Katzung BG, Trevor AJ. Basic & Clinical Pharmacology. 15th ed. McGraw-Hill; 2022. Insulin & oral hypoglycemic agents.
- Ritter JM, Flower R, Henderson G, et al. Rang & Dale’s Pharmacology. 10th ed. London: Elsevier; 2023. Antidiabetic drugs.
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.

