Antimicrobial agents can be broadly classified into six main categories: antibiotics, antivirals, antifungals, antiprotozoals, anthelmintics, and antiseptics.
- Antibiotics:
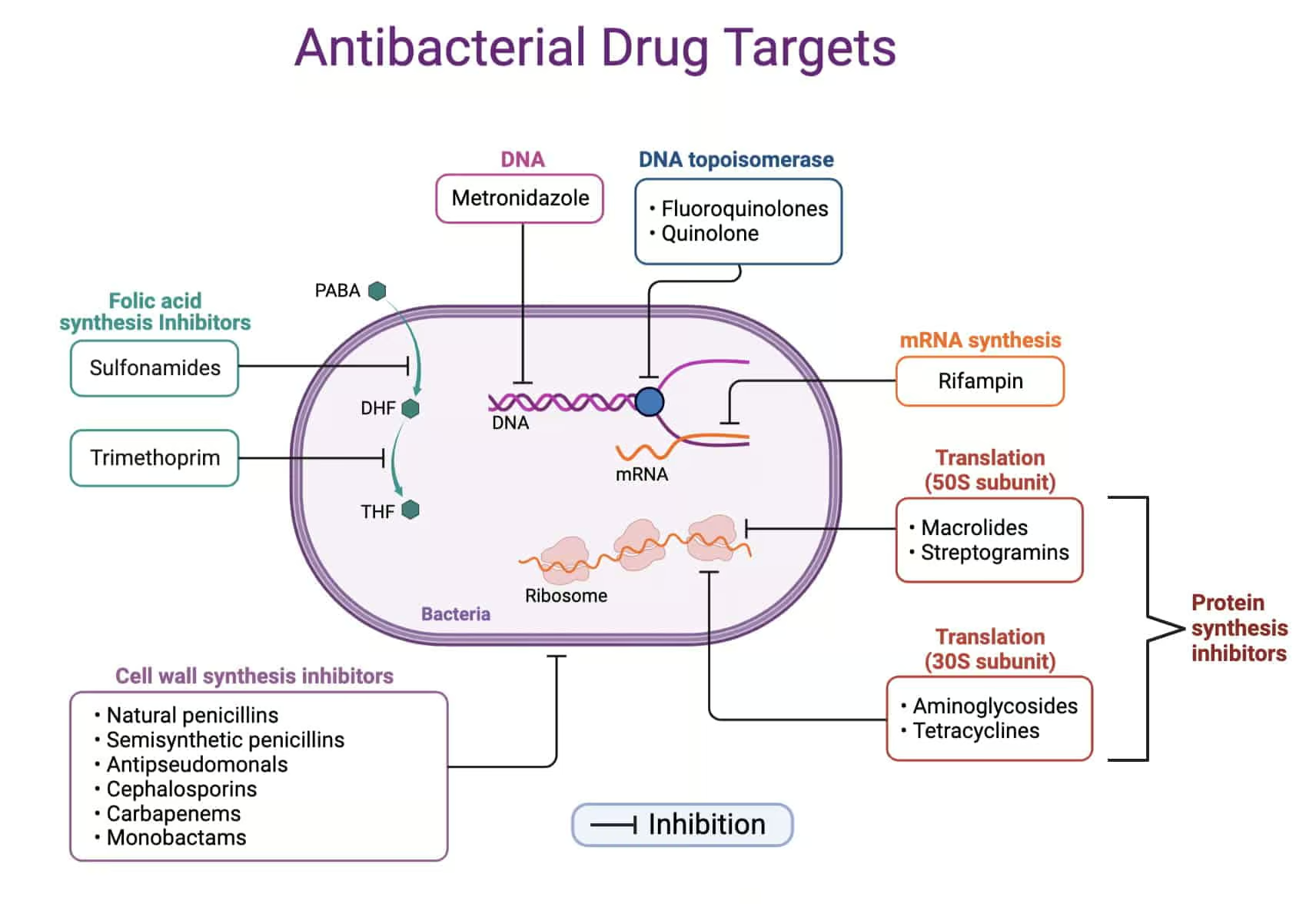
Antibiotics can be classified into several classes based on their chemical structure, mechanism of action, and spectrum of activity. Some of the major classes include:
a. Beta-lactams:
Examples: Penicillins (e.g., amoxicillin, penicillin G), cephalosporins (e.g., cephalexin, ceftriaxone), and carbapenems (e.g., imipenem, meropenem).
Mechanism of action: Inhibit bacterial cell wall synthesis by binding to penicillin-binding proteins.
Pharmacological actions: Bactericidal.
Uses: Respiratory tract infections, urinary tract infections, skin infections, and bacterial meningitis.
Adverse effects: Hypersensitivity reactions, diarrhea, nephrotoxicity (carbapenems).
Contraindications: Allergy to beta-lactam antibiotics.
b. Tetracyclines:
Examples: Tetracycline, doxycycline, and minocycline.
Mechanism of action: Inhibit protein synthesis by binding to the 30S ribosomal subunit.
Pharmacological actions: Bacteriostatic. Uses: Acne, respiratory tract infections, and Lyme disease.
Adverse effects: Gastrointestinal disturbances, photosensitivity, and tooth discoloration in children.
Contraindications: Pregnancy, lactation, and children under 8 years old.
c. Macrolides:
Examples: Erythromycin, azithromycin, and clarithromycin.
Mechanism of action: Inhibit protein synthesis by binding to the 50S ribosomal subunit.
Pharmacological actions: Bacteriostatic, bactericidal at high concentrations.
Uses: Respiratory tract infections, skin infections, and sexually transmitted infections.
Adverse effects: Gastrointestinal disturbances, QT interval prolongation, and hepatotoxicity.
Contraindications: Allergy to macrolides, severe liver impairment, and concomitant use of certain medications that prolong the QT interval.
d. Fluoroquinolones:
Examples: Ciprofloxacin, levofloxacin, and moxifloxacin.
Mechanism of action: Inhibit bacterial DNA gyrase and topoisomerase IV, enzymes involved in DNA replication and transcription.
Pharmacological actions: Bactericidal.
Uses: Urinary tract infections, respiratory tract infections, and gastrointestinal infections.
Adverse effects: Gastrointestinal disturbances, tendonitis, tendon rupture, QT interval prolongation, and central nervous system effects (e.g., headache, dizziness).
Contraindications: Allergy to fluoroquinolones, pregnancy, lactation, and children under 18 years old.
e. Aminoglycosides:
Examples: Gentamicin, amikacin, and tobramycin.
Mechanism of action: Inhibit protein synthesis by binding to the 30S ribosomal subunit. Pharmacological actions: Bactericidal.
Pharmacokinetics: Highly polar drugs, not absorbed by oral route. Therefore, these are administered parenterally and topically.
Uses: Severe Gram-negative infections and as an adjunctive therapy in endocarditis.
Adverse effects: Nephrotoxicity, ototoxicity, and neuromuscular blockade.
Contraindications: Hypersensitivity to aminoglycosides, severe renal impairment, and myasthenia gravis.
f. Sulfonamides and trimethoprim:
Examples: Sulfamethoxazole, sulfadiazine, and trimethoprim-sulfamethoxazole (co-trimoxazole).
Mechanism of action: Sulfonamides inhibit dihydropteroate synthase, and trimethoprim inhibits dihydrofolate reductase. Both enzymes are involved in the bacterial synthesis of folic acid.
Pharmacological actions: Bacteriostatic.
Uses: Urinary tract infections, respiratory tract infections, and certain types of gastrointestinal infections.
Adverse effects: Hypersensitivity reactions, gastrointestinal disturbances, hemolytic anemia, and crystalluria.
Contraindications: Allergy to sulfonamides or trimethoprim, severe liver or renal impairment, and pregnancy (especially during the first trimester and near term).
g. Glycopeptides:
Examples: Vancomycin and teicoplanin.
Mechanism of action: Inhibit bacterial cell wall synthesis by binding to the D-alanyl-D-alanine terminus of the peptidoglycan precursor.
Pharmacological actions: Bactericidal.
Uses: Severe Gram-positive infections, including methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile infections.
Adverse effects: Nephrotoxicity, ototoxicity, and infusion-related reactions (e.g., “red man syndrome”).
Contraindications: Allergy to glycopeptides and severe renal impairment.
h. Oxazolidinones:
Examples: Linezolid and tedizolid.
Mechanism of action: Inhibit protein synthesis by binding to the 50S ribosomal subunit.
Pharmacological actions: Bacteriostatic.
Uses: Skin and soft tissue infections, pneumonia, and infections caused by vancomycin-resistant enterococci (VRE).
Adverse effects: Gastrointestinal disturbances, myelosuppression (particularly thrombocytopenia), and peripheral neuropathy.
Contraindications: Hypersensitivity to oxazolidinones and concomitant use of monoamine oxidase inhibitors (MAOIs).
i. Lincosamides:
Examples: Clindamycin and lincomycin.
Mechanism of action: Inhibit protein synthesis by binding to the 50S ribosomal subunit.
Pharmacological actions: Bacteriostatic, bactericidal at high concentrations.
Uses: Skin and soft tissue infections, particularly those caused by anaerobic bacteria.
Adverse effects: Gastrointestinal disturbances, pseudomembranous colitis (C. difficile infection), and hypersensitivity reactions.
Contraindications: Hypersensitivity to lincosamides and a history of C. difficile infection.
j. Nitroimidazoles:
Examples: Metronidazole and tinidazole.
Mechanism of action: Disruption of bacterial DNA structure through the formation of nitroso radicals.
Pharmacological actions: Bactericidal.
Uses: Anaerobic bacterial infections, protozoal infections (e.g., giardiasis, trichomoniasis), and Clostridium difficile infections.
Adverse effects: Gastrointestinal disturbances, metallic taste, peripheral neuropathy, and disulfiram-like reaction with alcohol.
Contraindications: Hypersensitivity to nitroimidazoles, first trimester of pregnancy, and consumption of alcohol during treatment and up to 48 hours after completion.
k. Polymyxins:
Examples: Polymyxin B and colistin (polymyxin E). Mechanism of action: Disruption of bacterial cell membrane integrity by interacting with lipopolysaccharide.
Pharmacological actions: Bactericidal.
Uses: Multidrug-resistant Gram-negative infections, particularly those caused by Pseudomonas aeruginosa and Acinetobacter species.
Adverse effects: Nephrotoxicity, neurotoxicity (including neuromuscular blockade), and allergic reactions.
Contraindications: Hypersensitivity to polymyxins and severe renal impairment.
l. Streptogramins:
Examples: Quinupristin-dalfopristin (Synercid).
Mechanism of action: Inhibit bacterial protein synthesis by binding to the 50S ribosomal subunit.
Pharmacological actions: Bacteriostatic individually, bactericidal in combination.
Uses: Skin and soft tissue infections, particularly those caused by methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococcus faecium (VREF).
Adverse effects: Gastrointestinal disturbances, infusion-related reactions, and arthralgia or myalgia.
Contraindications: Hypersensitivity to streptogramins and concomitant use of certain medications that may cause drug-drug interactions.
m. Cyclic lipopeptides:
Example: Daptomycin.
Mechanism of action: Disruption of bacterial cell membrane integrity by binding to membrane phospholipids and forming pores.
Pharmacological actions: Bactericidal.
Uses: Skin and soft tissue infections, bacteremia, and right-sided endocarditis caused by Gram-positive bacteria, including MRSA and VRE.
Adverse effects: Gastrointestinal disturbances, myopathy (elevated creatine phosphokinase levels), and eosinophilic pneumonia.
Contraindications: Hypersensitivity to daptomycin and use in pulmonary infections (due to inactivation by lung surfactant).
n. Monobactams:
Example: Aztreonam.
Mechanism of action: Inhibit bacterial cell wall synthesis by binding to penicillin-binding proteins.
Pharmacological actions: Bactericidal.
Uses: Gram-negative infections, particularly in patients with severe penicillin or cephalosporin allergies.
Adverse effects: Gastrointestinal disturbances, hypersensitivity reactions, and neurotoxicity (e.g., seizures) with high doses.
Contraindications: Hypersensitivity to aztreonam.
- Antivirals:
Antiviral agents can be classified into several categories based on the type of virus they target and their mechanism of action. Some of the major classes include:
a. Antiviral agents for herpesviruses:
Examples: Acyclovir, valacyclovir, and famciclovir.
Mechanism of action: Inhibit viral DNA polymerase, preventing the synthesis of viral DNA.
Pharmacological actions: Virustatic.
Uses: Herpes simplex virus (HSV) infections, varicella-zoster virus (VZV) infections, and prophylaxis in immunocompromised patients.
Adverse effects: Gastrointestinal disturbances, headache, and nephrotoxicity (with high doses or intravenous administration).
Contraindications: Hypersensitivity to the specific antiviral agent and severe renal dysfunction.
b. Nucleoside and nucleotide reverse transcriptase inhibitors (NRTIs):
Examples: Zidovudine, lamivudine, and tenofovir.
Mechanism of action: Inhibit viral reverse transcriptase, preventing the synthesis of viral DNA from RNA templates. Pharmacological actions: Virustatic.
Uses: Human immunodeficiency virus (HIV) infection and certain hepatitis B infections.
Adverse effects: Gastrointestinal disturbances, myelosuppression, anaemais, lactic acidosis, and peripheral neuropathy.
Contraindications: Hypersensitivity to the specific NRTI and certain drug-drug interactions.
c. Non-nucleoside reverse transcriptase inhibitors (NNRTIs):
Examples: Efavirenz, nevirapine, and rilpivirine.
Mechanism of action: Inhibit viral reverse transcriptase by binding to an allosteric site.
Pharmacological actions: Virustatic.
Uses: HIV infection.
Adverse effects: Gastrointestinal disturbances, rash, hepatotoxicity, and central nervous system effects (e.g., dizziness, insomnia).
Contraindications: Hypersensitivity to the specific NNRTI and certain drug-drug interactions.
d. Protease inhibitors (PIs):
Examples: Atazanavir, darunavir, and lopinavir/ritonavir.
Mechanism of action: Inhibit viral protease, preventing the cleavage of viral polyprotein precursors into functional proteins.
Pharmacological actions: Virustatic.
Uses: HIV infection.
Adverse effects: Gastrointestinal disturbances, hyperlipidemia, insulin resistance, and lipodystrophy.
Contraindications: Hypersensitivity to the specific PI and certain drug-drug interactions.
e. Integrase strand transfer inhibitors (INSTIs):
Examples: Raltegravir, dolutegravir, and bictegravir.
Mechanism of action: Inhibit the integration of viral DNA into the host cell genome.
Pharmacological actions: Virustatic.
Uses: HIV infection.
Adverse effects: Gastrointestinal disturbances, headache, and hypersensitivity reactions.
Contraindications: Hypersensitivity to the specific INSTI and certain drug-drug interactions.
f. Neuraminidase inhibitors:
Examples: Oseltamivir, zanamivir, and peramivir.
Mechanism of action: Inhibit viral neuraminidase, preventing the release of new virions from infected cells.
Pharmacological actions: Virustatic.
Uses: Influenza A and B infections. Adverse effects: Gastrointestinal disturbances, headache, and bronchospasm (zanamivir).
Contraindications: Hypersensitivity to the specific neuraminidase inhibitor and certain underlying respiratory conditions (e.g., asthma or chronic obstructive pulmonary disease) for Zanamivir.
g. Direct-acting antivirals (DAAs) for hepatitis C:
Examples: Sofosbuvir, ledipasvir, and velpatasvir.
Mechanism of action: Target various stages of the hepatitis C virus (HCV) life cycle, including viral replication, protease activity, and viral assembly. Pharmacological actions: Virustatic.
Uses: Chronic hepatitis C infection.
Adverse effects: Gastrointestinal disturbances, headache, and fatigue.
Contraindications: Hypersensitivity to the specific DAA and certain drug-drug interactions.
Disclaimer: This article is for informational purposes only and should not be taken as medical advice. Always consult with a healthcare professional before making any decisions related to medication or treatment.
- Antifungals:
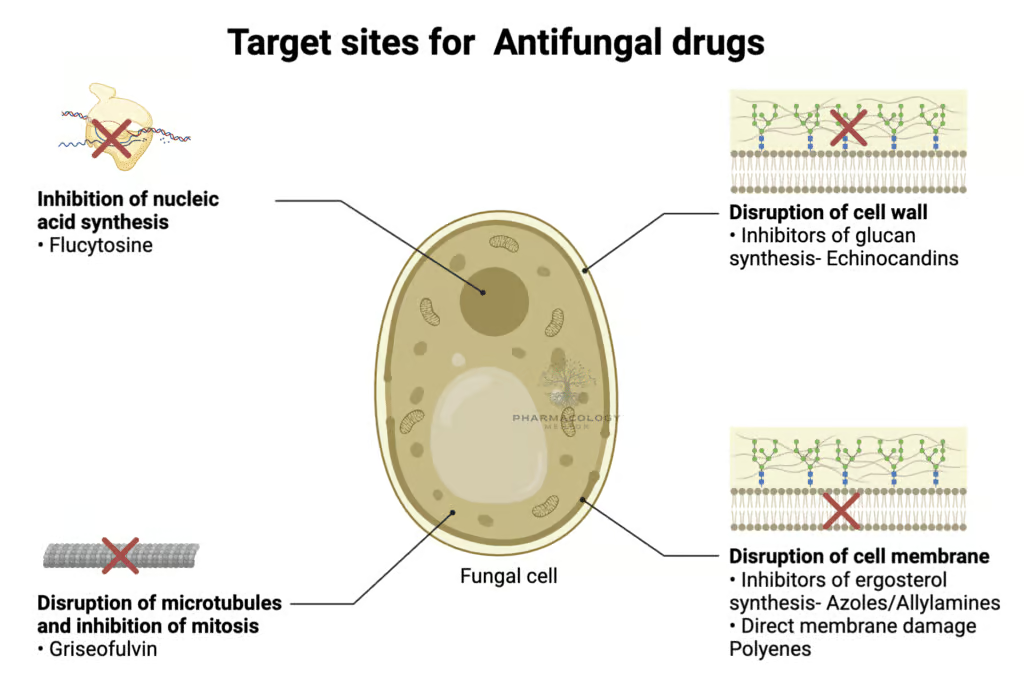
Antifungal agents can be classified into several categories based on their mechanism of action. Some of the major classes include:
a. Azoles:
Examples: Fluconazole, itraconazole, and voriconazole.
Mechanism of action: Inhibit fungal ergosterol synthesis by inhibiting the enzyme lanosterol 14α-demethylase.
Pharmacological actions: Fungistatic.
Uses: Candida infections, Aspergillus infections, and dermatophyte infections.
Adverse effects: Gastrointestinal disturbances, hepatotoxicity, and drug-drug interactions.
Contraindications: Hypersensitivity to azoles and certain drug-drug interactions.
b. Polyenes:
Examples: Amphotericin B and nystatin.
Mechanism of action: Bind to ergosterol in the fungal cell membrane, leading to pore formation and cell leakage.
Pharmacological actions: Fungicidal.
Uses: Systemic fungal infections (amphotericin B) and oral or topical candidiasis (nystatin).
Adverse effects: Nephrotoxicity, infusion-related reactions, and electrolyte imbalances (amphotericin B); gastrointestinal disturbances (nystatin).
Contraindications: Hypersensitivity to polyenes and severe renal impairment (amphotericin B).
c. Echinocandins:
Examples: Caspofungin, micafungin, and anidulafungin.
Mechanism of action: Inhibit fungal cell wall synthesis by inhibiting the enzyme β-(1,3)-D-glucan synthase.
Pharmacological actions: Fungicidal.
Uses: Invasive candidiasis and aspergillosis.
Adverse effects: Gastrointestinal disturbances, headache, and infusion-related reactions.
Contraindications: Hypersensitivity to echinocandins.
d. Allylamines:
Example: Terbinafine.
Mechanism of action: Inhibit fungal ergosterol synthesis by inhibiting the enzyme squalene epoxidase. Pharmacological actions: Fungicidal.
Uses: Dermatophyte infections (e.g., tinea pedis, tinea corporis, and onychomycosis).
Adverse effects: Gastrointestinal disturbances, hepatotoxicity, and taste disturbances.
Contraindications: Hypersensitivity to allylamines and severe liver impairment.
- Antiprotozoal agents:
Antiprotozoal agents can be classified into several categories based on the protozoan they target. Some of the major classes include:
a. Antimalarials:
For detailed notes and key points on antimalarial drugs, click here:
Examples: Chloroquine, mefloquine, and artemisinin derivatives.
Mechanism of action: Varies depending on the agent but generally involves disruption of parasite metabolism, replication, or invasion.
Pharmacological actions: Protozoastatic.
Uses: Malaria treatment and prophylaxis.
Adverse effects: Gastrointestinal disturbances, headache, and central nervous system effects (e.g., dizziness, seizures).
Contraindications: Hypersensitivity to the specific antimalarial agent and certain underlying medical conditions (e.g., epilepsy, heart conduction abnormalities).
b. Nitroimidazoles (also listed under antibiotics):
Examples: Metronidazole and tinidazole.
Mechanism of action: Disruption of protozoal DNA structure through the formation of nitroso radicals. Pharmacological actions: Protozoacidal.
Uses: Giardiasis, trichomoniasis, and amoebic dysentery.
Adverse effects: Gastrointestinal disturbances, metallic taste, peripheral neuropathy, and disulfiram-like reaction with alcohol.
Contraindications: Hypersensitivity to nitroimidazoles, first trimester of pregnancy, and consumption of alcohol during treatment and up to 48 hours after completion.
c. Antitrypanosomal agents:
Examples: Suramin, pentamidine, and nifurtimox.
Mechanism of action: Varies depending on the agent but generally involves disruption of parasite metabolism, replication, or invasion.
Pharmacological actions: Protozoacidal. Uses: African trypanosomiasis (sleeping sickness) and American trypanosomiasis (Chagas disease).
Adverse effects: Gastrointestinal disturbances, nephrotoxicity, and central nervous system effects (e.g., dizziness, seizures).
Contraindications: Hypersensitivity to the specific antitrypanosomal agent and certain underlying medical conditions (e.g., renal or hepatic impairment).
d. Antileishmanial agents:
Examples: Sodium stibogluconate, miltefosine, and amphotericin B (also listed under antifungals).
Mechanism of action: Varies depending on the agent but generally involves disruption of parasite metabolism, replication, or invasion.
Pharmacological actions: Protozoacidal. Uses: Leishmaniasis (cutaneous, mucocutaneous, and visceral forms).
Adverse effects: Gastrointestinal disturbances, hepatotoxicity, nephrotoxicity (amphotericin B), and pancreatitis (miltefosine).
Contraindications: Hypersensitivity to the specific antileishmanial agent, pregnancy (miltefosine), and severe renal or hepatic impairment (amphotericin B).
- Antihelminthic agents:
Antihelminthic agents can be classified into several categories based on the type of helminth they target. Some of the major classes include:
a. Benzimidazoles:
Examples: Albendazole and mebendazole.
Mechanism of action: Inhibit microtubule synthesis in helminths, impairing glucose uptake and depleting energy reserves.
Pharmacological actions: Helminthicidal. Uses: Intestinal nematode infections (e.g., roundworms, hookworms, whipworms) and tissue nematode infections (e.g., cysticercosis, hydatid disease).
Adverse effects: Gastrointestinal disturbances, headache, and reversible bone marrow suppression (with prolonged use).
Contraindications: Hypersensitivity to benzimidazoles and first trimester of pregnancy.
b. Ivermectin:
Mechanism of action: Increases the permeability of helminth cell membranes to chloride ions, leading to paralysis and death of the parasites. Pharmacological actions: Helminthicidal.
Uses: Intestinal nematode infections (e.g., strongyloidiasis, ascariasis), tissue nematode infections (e.g., onchocerciasis, lymphatic filariasis), and ectoparasitic infections (e.g., scabies, lice).
Adverse effects: Gastrointestinal disturbances, headache, and Mazzotti reaction (in patients with onchocerciasis).
Contraindications: Hypersensitivity to ivermectin and certain underlying medical conditions (e.g., meningitis, severe central nervous system disorders).
c. Praziquantel:
Mechanism of action: Increases the permeability of helminth cell membranes to calcium ions, leading to contraction, paralysis, and death of the parasites.
Pharmacological actions: Helminthicidal.
Uses: Trematode (fluke) infections (e.g., schistosomiasis, liver flukes) and cestode (tapeworm) infections (e.g., taeniasis, cysticercosis).
Adverse effects: Gastrointestinal disturbances, headache, dizziness, and allergic reactions.
Contraindications: Hypersensitivity to praziquantel and certain underlying medical conditions (e.g., ocular cysticercosis).
d. Niclosamide:
Mechanism of action: Inhibits anaerobic respiration and ATP production in cestodes, leading to paralysis and death of the parasites.
Pharmacological actions: Cestodicidal.
Uses: Cestode (tapeworm) infections (e.g., taeniasis, diphyllobothriasis).
Adverse effects: Gastrointestinal disturbances, dizziness, and rash.
Contraindications: Hypersensitivity to niclosamide.
e. Pyrantel pamoate:
Mechanism of action: Acts as a neuromuscular blocker, causing paralysis and expulsion of the worms from the gastrointestinal tract.
Pharmacological actions: Helminthicidal.
Uses: Intestinal nematode infections (e.g., roundworms, hookworms, pinworms).
Adverse effects: Gastrointestinal disturbances, headache, and dizziness.
Contraindications: Hypersensitivity to pyrantel pamoate and severe hepatic dysfunction.
Antitubercular agents can be classified into several categories based on their mechanism of action and their role in the treatment of tuberculosis (TB). Some of the major classes include:
a. First-line antitubercular agents:
Examples: Isoniazid, rifampin, pyrazinamide, and ethambutol.
Mechanism of action: Varies depending on the agent but generally involves disruption of bacterial cell wall synthesis, protein synthesis, or metabolic pathways.
Pharmacological actions: Bactericidal (isoniazid, rifampin, pyrazinamide) and bacteriostatic (ethambutol).
Uses: Active tuberculosis and latent TB infection (isoniazid).
Adverse effects: Hepatotoxicity (isoniazid, rifampin, pyrazinamide), peripheral neuropathy (isoniazid), gastrointestinal disturbances, and optic neuritis (ethambutol).
Contraindications: Hypersensitivity to the specific antitubercular agent, severe hepatic dysfunction, and optic neuritis (ethambutol).
b. Second-line antitubercular agents:
Examples: Streptomycin, amikacin, kanamycin, capreomycin, levofloxacin, moxifloxacin, ethionamide, and cycloserine.
Mechanism of action: Varies depending on the agent but generally involves disruption of bacterial protein synthesis or metabolic pathways.
Pharmacological actions: Bactericidal (aminoglycosides, fluoroquinolones) and bacteriostatic (ethionamide, cycloserine).
Uses: Multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB).
Adverse effects: Ototoxicity and nephrotoxicity (aminoglycosides, capreomycin), gastrointestinal disturbances, hepatotoxicity (ethionamide), and central nervous system effects (cycloserine).
Contraindications: Hypersensitivity to the specific antitubercular agent, severe renal dysfunction, and certain underlying medical conditions (e.g., epilepsy, depression).
Managing infections caused by various microbes involves using antimicrobial agents that target specific pathogens or their metabolic pathways. Proper selection of antimicrobial agents, taking into consideration factors such as their mechanisms of action, pharmacological actions, uses, adverse effects, and contraindications, can lead to effective treatment and minimize the risk of side effects and the development of antimicrobial resistance. Additionally, educating patients about the appropriate use of antimicrobial agents and the importance of adherence to the prescribed treatment regimen is crucial to ensure the best possible outcomes.
Disclaimer: This article is for informational purposes only and should not be taken as medical advice. Always consult with a healthcare professional before making any decisions related to medication or treatment.