Introduction
Angina pectoris, often referred to simply as angina, is chest pain or discomfort that arises when the myocardial oxygen supply is insufficient to meet the heart’s metabolic demands. As a cardinal manifestation of coronary artery disease (CAD), angina affects millions of people worldwide, posing a significant burden on healthcare systems and patient quality of life. Chronic stable angina typically presents as discomfort precipitated by exertion or stress, relieved by rest or nitroglycerin, whereas unstable angina indicates a more dangerous form of ischemic heart disease that demands urgent medical attention.
Pharmacotherapy for angina pectoris involves a multi-pronged approach aimed at reducing oxygen demand, improving coronary blood flow, and minimizing atherosclerotic progression. Clinicians often combine lifestyle modifications with various classes of medication to ensure effective and enduring symptom control. This article provides a thorough exploration of antianginal pharmacotherapy, discussing mechanisms of action, indications, side effect profiles, and the evidence base supporting each class of agent, with references to well-established textbooks.
Understanding Angina Pectoris
Angina, derived from the Latin word for “strangling,” manifests as a tightening or pressure-like sensation in the chest. Pathophysiologically, it is caused by an imbalance between myocardial oxygen supply (dependent on coronary blood flow and oxygen content) and oxygen demand (determined by heart rate, contractility, and wall tension) (Braunwald, 2021). When coronary arteries narrowed by atherosclerosis cannot supply enough oxygenated blood to meet metabolic requirements—particularly during exertion—ischemia ensues, and patients typically experience angina.
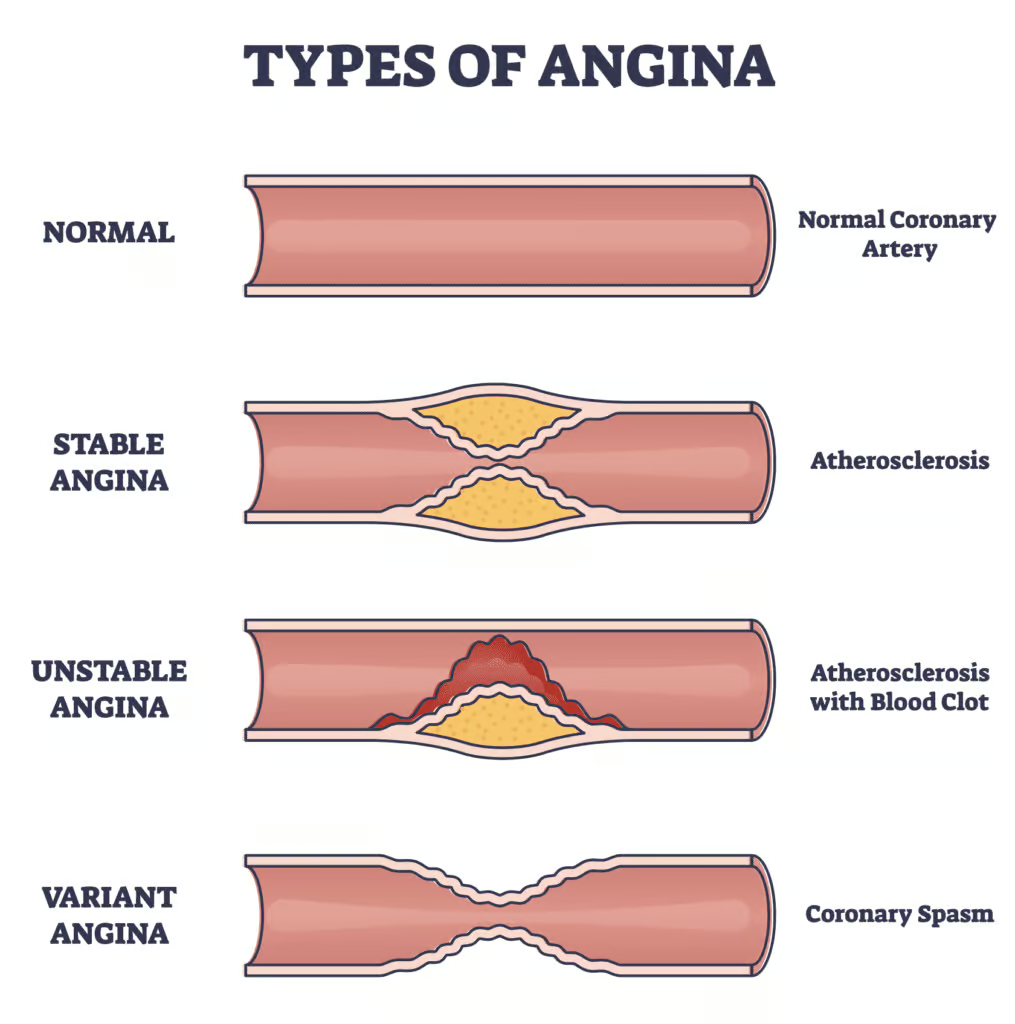
Types of Angina
- Stable (Chronic) Angina: Characterized by predictable chest pain on exertion or emotional stress, usually relieved by rest or sublingual nitroglycerin.
- Unstable Angina (UA): Denotes an acute change in frequency or intensity of anginal episodes, often occurring at rest. UA is a form of acute coronary syndrome requiring urgent medical evaluation.
- Prinzmetal’s (Variant) Angina: Caused by coronary vasospasm, often presenting with transient ST-segment elevation. This variant tends to occur at rest and responds effectively to calcium channel blockers and nitrates.
Stress testing, electrocardiography, and, in some cases, cardiac catheterization help confirm the diagnosis and guide treatment decisions. The overarching management goal is to mitigate ischemia, relieve symptoms, and improve long-term cardiovascular outcomes.
Goals of Pharmacotherapy in Angina
The primary objectives of pharmacotherapy are:
- Improvement of Myocardial Oxygen Balance: By reducing myocardial oxygen demand and/or increasing coronary blood flow.
- Symptom Relief: Minimizing the frequency and severity of anginal episodes.
- Prevention of Cardiac Events: Reducing the risk of myocardial infarction, heart failure, and sudden cardiac death.
- Enhancement of Quality of Life: Enabling patients to engage in normal activities with minimal limitation.
Pharmacological approaches aim to:
- Decrease heart rate, contractility, and other contributors to myocardial workload.
- Dilate coronary vasculature to improve blood flow in ischemic regions.
- Prevent platelet aggregation and thrombosis.
- Slow the progression of atherosclerosis by modifying lipid profiles and healing endothelium.
Major Classes of Antianginal Medications
1. Beta-Adrenergic Blockers
Beta-blockers (β-blockers) are among the first-line therapies for chronic stable angina. By inhibiting β-adrenergic receptors, they decrease heart rate, contractility, and blood pressure, effectively reducing myocardial oxygen demand (Brunton, 2022).
Mechanism of Action
β1 receptors predominate in the heart, where their stimulation leads to increased heart rate and contractility. β-blockers counteract these effects by preventing catecholamines (e.g., norepinephrine, epinephrine) from binding to the β1 receptors. Heart rate, contractility, and conduction velocity all decline, translating into a reduced oxygen requirement for cardiac muscle.
Common Beta-Blockers
- Metoprolol (β1-selective)
- Bisoprolol (β1-selective)
- Atenolol (β1-selective)
- Propranolol (non-selective)
- Carvedilol (non-selective, also blocks α1)
Clinical Usage
- Stable Angina: Beta-blockers are standard for rate control, symptom alleviation, and limiting ischemic episodes.
- Post-MI Management: They lower mortality in patients who have suffered myocardial infarction.
- Hypertensive Patients: Particularly beneficial in those with hypertension coexisting with angina.
Side Effects
- Bradycardia and potential heart block
- Fatigue and Exercise Intolerance
- Bronchospasm (especially with non-selective β-blockers in asthmatic patients)
- Exacerbation of Peripheral Vascular Disease
Because β-blockers also modulate the conduction system, abrupt withdrawal may precipitate rebound tachycardia or ischemia. Gradual dose tapering is critical.
2. Calcium Channel Blockers
Calcium channel blockers (CCBs) are a heterogeneous group subdivided into dihydropyridines (e.g., amlodipine, nifedipine) and non-dihydropyridines (e.g., verapamil, diltiazem). They reduce calcium influx across cardiac and smooth muscle cells, diminishing contractility and promoting vasodilation (Katzung, 2021).
Mechanism of Action
- Dihydropyridines primarily target vascular smooth muscle, leading to arterial dilation and a drop in systemic vascular resistance (afterload).
- Non-dihydropyridines also reduce heart rate and contractility by inhibiting calcium entry in the sinoatrial (SA) and atrioventricular (AV) nodes.
Clinical Usage
- Prinzmetal’s Angina: Calcium channel blockers of both subtypes are especially effective for vasospastic angina.
- Stable Angina: CCBs provide additional symptomatic relief or serve as an alternative when beta-blockers are contraindicated.
- Hypertension + Angina: Agents like amlodipine address both conditions concurrently.
Side Effects
- Dihydropyridines:Peripheral edema, headache, flushing, reflex tachycardia (especially short-acting formulations like immediate-release nifedipine).
- Non-Dihydropyridines: Bradycardia, AV nodal blockade, constipation (particularly verapamil), and additive negative inotropy.
Combining β-blockers with non-dihydropyridines requires caution due to a potential for excessive bradycardia and AV block.
3. Nitrates
Nitrates have long been a cornerstone of angina management. Nitroglycerin (glyceryl trinitrate) and related compounds act by releasing nitric oxide (NO), prompting vasodilation of both veins and arteries.
Mechanism of Action
Nitric oxide activates guanylyl cyclase, raising cGMP levels, which in turn promote dephosphorylation of myosin light chains leading to smooth muscle relaxation (Braunwald, 2021). Venodilation is most prominent, reducing venous return (preload) and thereby lowering myocardial wall stress and oxygen consumption. At higher doses, nitrates dilate arterial vessels (reducing afterload). Additionally, nitrates can help alleviate coronary vasospasm.
Dosage Forms
- Sublingual Nitroglycerin Tablets/Spray: Rapid onset for acute angina relief.
- Transdermal Patch or Ointment: Provides longer-duration prophylaxis.
- Oral Isosorbide Mononitrate/Isosorbide Dinitrate: Prophylactic management of chronic angina.
Tolerance and Administration
Continuous nitrate exposure can induce tolerance. Patients are instructed to have a nitrate-free interval (generally at night) to restore sensitivity. Timing of patches or long-acting formulations is arranged to maximize efficacy during daytime hours when angina episodes are more frequent.
Side Effects
- Headaches: Especially upon initiation due to vasodilation.
- Orthostatic Hypotension: Can lead to reflex tachycardia.
- Flushing
- Interaction with PDE5 Inhibitors: Potentially life-threatening hypotension occurs if nitrates are combined with sildenafil, tadalafil, or vardenafil used for erectile dysfunction.
Nitrates remain highly effective for rapid symptomatic relief and prevention of ischemic episodes when combined with β-blockers or calcium channel blockers.
4. Ranolazine
Ranolazine is a relatively newer agent that helps reduce angina symptoms without impacting heart rate or blood pressure to a significant degree.
Mechanism of Action
Ranolazine inhibits the late inward sodium current (I_Na) in cardiac myocytes, which indirectly reduces intracellular calcium and, consequently, diastolic wall tension. By optimizing myocardial relaxation, ranolazine lowers oxygen demand (Brunton, 2022).
Indications and Efficacy
- Chronic Stable Angina: Added to standard therapy (e.g., β-blockers, nitrates) to further reduce angina frequency and improve exercise tolerance.
- Preserved Blood Pressure and Heart Rate: Ranolazine may be of use in patients who develop intolerable hypotension or bradycardia with other agents.
Side Effects
- QT Prolongation: Caution with concurrent QT-prolonging medications. Monitoring with periodic electrocardiograms is essential in susceptible patients.
- Dizziness, Headache, Constipation: Relatively common but generally mild.
- Drug Interactions: Metabolized by CYP3A4, so concurrent strong inhibitors (e.g., certain antifungals, macrolide antibiotics) must be avoided or used cautiously.
Ranolazine aligns well with other antianginal agents, offering an option for patients with refractory angina or those who cannot tolerate higher doses of first-line drugs.
5. Antiplatelet Therapy
Platelet aggregation plays a pivotal role in coronary thrombosis, especially in unstable angina. Although not strictly “antianginal” in the hemodynamic sense, antiplatelet agents are integral for preventing acute coronary events.
Aspirin
- Mechanism: Irreversible inhibition of cyclooxygenase-1 (COX-1) curtails thromboxane A2 synthesis, reducing platelet aggregation.
- Usage: Low-dose aspirin (75-100 mg daily) is recommended for most patients with coronary artery disease.
- Side Effects: Gastrointestinal irritation, bleeding risk, rare hypersensitivity.
P2Y12 Inhibitors
- Clopidogrel, Prasugrel, Ticagrelor: Block ADP-mediated platelet aggregation.
- Often combined with aspirin (dual antiplatelet therapy) for high-risk patients or after stent placement.
By thwarting thrombus formation, antiplatelet agents prevent progression from stable angina to unstable presentations or myocardial infarction.
6. Statins and Other Lipid-Lowering Therapies
While statins do not provide immediate angina relief, they significantly reduce atherosclerotic progression, improve endothelial function, and stabilize plaques (Katzung, 2021).
Mechanism of Action
Statins (e.g., atorvastatin, rosuvastatin) inhibit HMG-CoA reductase, the enzyme crucial for endogenous cholesterol synthesis, thereby lowering LDL cholesterol. Reduced LDL levels slow plaque accumulation and can help regress existing atherosclerotic lesions over time.
Evidence for Use
Landmark trials have consistently demonstrated that statins reduce cardiovascular events, total mortality, and the need for revascularization in patients with coronary artery disease. For anyone with angina (indicative of underlying CAD), statin therapy is generally recommended unless contraindicated.
Side Effects
- Myalgias, Myopathy: Muscle aches, potentially rising to rhabdomyolysis in rare cases.
- Liver Function Test (LFT) Abnormalities: Periodic monitoring is advised.
- New-Onset Diabetes Risk: A slight increase in incidence among susceptible individuals.
In select patients, ezetimibe, PCSK9 inhibitors, or bile acid sequestrants are employed adjunctively if lipid goals remain unmet with statins alone.
Evidence-Based Combination Therapy
Optimal management of stable angina often requires multiple agents. For instance:
- β-blockers + Nitrates: β-blockers mitigate the nitrate-induced reflex tachycardia, and nitrates reduce preload. This synergy translates into enhanced symptom control.
- β-blockers + Dihydropyridine CCBs: The heart-rate-limiting effect of β-blockers balances out any reflex tachycardia caused by dihydropyridines.
- Ranolazine as an Add-On: Useful in patients unresponsive or intolerant to high doses of classic antianginals, offering further symptom relief without substantially affecting heart rate or blood pressure.
- Antiplatelet Agents + Statins: Address the atherosclerotic foundation of ischemic heart disease and reduce acute coronary event risk.
Treatment strategies must be individualized based on comorbidities, hemodynamic status, and patient preferences (Braunwald, 2021).
Unstable Angina and Acute Management
Unstable angina involves a heightened risk of acute myocardial infarction. In addition to optimizing antianginal therapies, the immediate management includes:
- Hospitalization and continuous ECG monitoring.
- High-intensity Statins for plaque stabilization.
- Dual Antiplatelet Therapy (e.g., aspirin + P2Y12 inhibitor) for thrombosis prevention.
- Anticoagulants (e.g., IV heparin, low-molecular-weight heparin, fondaparinux) to counter propagation of partial thromboses.
- Possible Revascularization (Percutaneous coronary intervention or coronary artery bypass grafting) depending on coronary anatomy and risk stratification.
Pharmacotherapy in unstable angina focuses on stabilizing plaque, preventing total occlusion, and controlling ischemic symptoms (Brunton, 2022).
Non-Pharmacological Management
Though pharmacological intervention remains integral, lifestyle modifications are crucial:
- Smoking Cessation: Smoking accelerates atherogenesis and antagonizes antianginal therapies.
- Diet and Exercise: A heart-healthy diet (low in saturated fats, high in fruits, vegetables, fibers) and consistent aerobic activity can mitigate angina severity.
- Weight Control: Obesity contributes to hypertension, insulin resistance, and increased cardiac workload.
- Stress Reduction: Behavioral therapies, relaxation techniques, and adequate sleep can help reduce episodes of stress-induced angina.
Invasive approaches like percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery may be indicated if medical therapy fails or coronary anatomy is highly obstructive.
Monitoring Treatment Efficacy
Regular follow-up visits allow clinicians to gauge symptom relief, medication tolerability, and overall cardiac risk:
- Symptom Assessment: Frequency, intensity, and threshold of angina episodes.
- Exercise Tolerance: Improvements noted through standardized exercise testing or daily activities.
- Vital Signs: Heart rate and blood pressure trending for dose adjustments.
- ECG Changes: ST-segment abnormalities, arrhythmias.
- Laboratory Tests: Lipid profile (for statin efficacy), renal and liver function, and potentially drug-specific monitoring (e.g., for ranolazine).
The concurrent presence of comorbidities (e.g., diabetes, hypertension, heart failure) dictates a need for comprehensive care.
Special Populations
1. Diabetic Patients
Diabetes accelerates CAD progression and can mask anginal pain (silent ischemia). Intensive glucose control, combined with a robust antianginal regimen (β-blockers, ACE inhibitors, statins, antiplatelets), drastically reduces cardiovascular complications.
2. Elderly Patients
Elderly individuals may exhibit reduced drug clearance and are more susceptible to orthostatic hypotension, bradyarrhythmias, and polypharmacy interactions. Start low and go slow when titrating.
3. Patients with Asthma/COPD
Non-selective β-blockers risk exacerbating bronchospasm. Cardio-selective (β1) blockers at low doses are relatively safer but still require caution.
4. Peripheral Arterial Disease (PAD)
Β-blockers occasionally worsen circulatory compromise in PAD. Careful monitoring of peripheral perfusion and symptomatology is warranted.Custom-tailoring regimens ensures optimal safety and efficacy in diverse clinical scenarios (Katzung, 2021).
Future Directions in Antianginal Pharmacotherapy
Advances in molecular cardiology and pharmacology have driven ongoing research into novel anti-ischemic treatments. Key areas of interest include:
- Ivabradine: Specifically lowers heart rate via blockade of the funny current (I_f) in the sinoatrial node without reducing contractility. It is used in heart failure and might be beneficial in select angina cases.
- Gene and Cell Therapies: Investigations continue for biological methods to promote angiogenesis or regenerate ischemic myocardium.
- PCSK9 Inhibitors: Already proven to significantly lower LDL cholesterol, they may improve ischemic outcomes when combined with other measures.
- Novel Antiplatelet/Antithrombotic Agents: Ongoing development aims at more potent, less bleeding-prone solutions for acute coronary syndromes.
- Ongoing Trials: Explore interventions targeting inflammatory pathways (e.g., IL-1 inhibitors) implicated in atherosclerosis and plaque instability.
These emerging therapies could transform angina management, offering more personalized and potent strategies with fewer side effects (Braunwald, 2021).
Clinical Pearls and Key Takeaways
- Lifestyle Modifications lay the foundation of angina management. Pharmacotherapy complements these changes.
- Beta-Blockers are typically first-line to reduce myocardial oxygen demand by lowering HR and contractility.
- Calcium Channel Blockers work well in vasospastic angina, as add-on therapy, or when β-blockers are intolerable or contraindicated.
- Nitrates remain indispensable for rapid relief and prophylaxis but require careful scheduling to avoid tolerance.
- Ranolazine offers a unique mechanism that can alleviate angina without causing bradycardia or hypotension.
- Antiplatelet Therapy (aspirin, P2Y12 inhibitors) is crucial for staving off acute coronary events.
- Statins enhance long-term outcomes by slowing atherosclerotic progression.
- Combination Therapies often provide synergistic benefits but must be calibrated to minimize adverse effects like excessive bradycardia or hypotension.
- Monitoring and follow-up are essential for adjusting therapy, ensuring compliance, and improving cardiovascular outcomes.
Ultimately, successful pharmacotherapy for angina pectoris revolves around personalized regimens that balance symptom control with prevention of adverse events, always underscored by comprehensive cardiovascular risk management.
Conclusion
Angina pectoris represents a significant clinical challenge arising from the intricate interplay of myocardial oxygen supply and demand. Its management requires a robust pharmacological approach combined with rigorous lifestyle modifications and potential revascularization procedures. Agents such as beta-blockers, calcium channel blockers, nitrates, ranolazine, and antiplatelets serve as the bedrock of therapy, each class addressing a unique facet of myocardial ischemia. Meanwhile, statins ensure that patients benefit from plaque stabilization and decreased atherosclerotic progression.
Optimal therapy begins with a thorough diagnostic workup to characterize disease severity and identify comorbidities. Then, clinicians tailor medications accordingly—often employing multiple classes simultaneously to balance efficacy with tolerability. Equally central, consistent follow-up and patient education about medication adherence, potential side effects, and red-flag symptoms serve as the foundation for successful long-term management.
As novel agents and innovative interventions continue to emerge—from refined lipid-lowering strategies to advanced molecular therapies—patients with angina pectoris will gain even more individualized and potent pathways to improved cardiac health. Nevertheless, the cornerstone of current best practice remains the time-tested synergy of established pharmacological classes, optimization of risk factors, and close, ongoing coordination between patients and their healthcare teams.
Book Citations
- Braunwald, E. (Ed.). (2021). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine (12th ed.). Philadelphia, PA: Elsevier.
- Brunton, L. (Ed.). (2022). Goodman & Gilman’s The Pharmacological Basis of Therapeutics (14th ed.). New York, NY: McGraw-Hill.
- Katzung, B.G. (Ed.). (2021). Basic & Clinical Pharmacology (15th ed.). New York, NY: McGraw-Hill.









