Scope and Definition
Anxiolytics are a class of pharmacological agents administered to treat pathological anxiety—a set of disorders characterized by excessive and unmanageable worry or fear. Anxiety may be generalized (GAD), situational (phobias), episodic (panic disorder), obsessive-compulsive (OCD), or post-traumatic (PTSD). Clinical management is driven by agent efficacy, risk profile, presence of comorbidities, and short- versus long-term goals.
Detailed Classification and Mechanisms
I. Benzodiazepines
- Major Drugs: Diazepam, Lorazepam, Alprazolam, Clonazepam, Oxazepam, Chlordiazepoxide
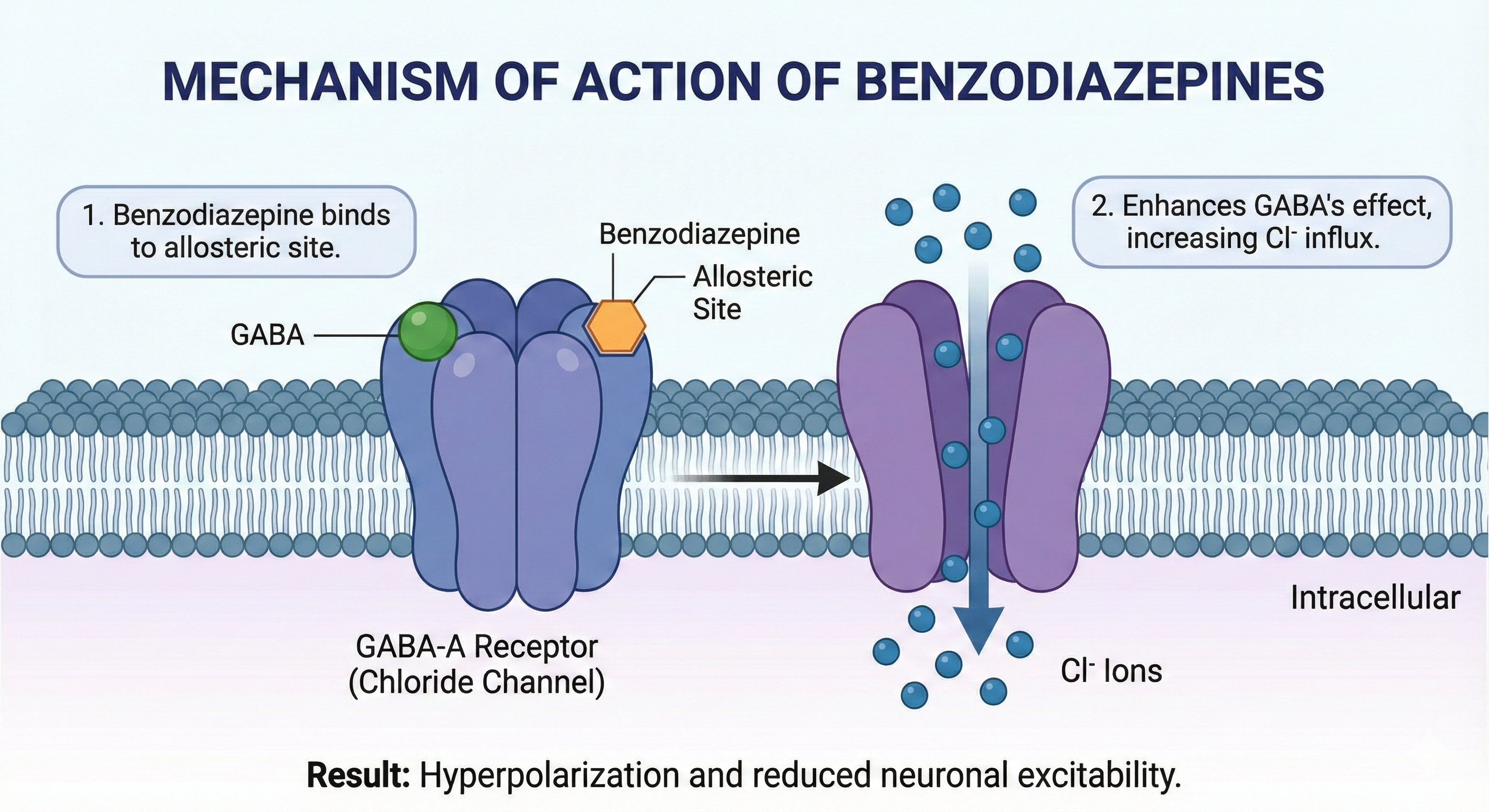
- Structural class: Allosteric modulators of GABAAA receptor (heteropentameric Cl−− channel).
- Mechanism: Bind at the interface of α and γ subunits on the GABAAA receptor, potentiate endogenous GABA’s chloride channel opening frequency. This hyperpolarizes neurons, resulting in reduced excitability.
- Pharmacokinetics:
- Absorption: Rapid and complete orally.
- Distribution: Lipophilic; cross the blood-brain barrier.
- Metabolism: Hepatic, some undergo active metabolite formation (e.g., diazepam), others (lorazepam, oxazepam) bypass phase I metabolism—safer in hepatic impairment.
- Elimination half-life: Ranges from <10 hrs (triazolam) to >40 hrs (diazepam, chlordiazepoxide).
- Clinical Use: Acute anxiety, panic attacks, muscle spasms, status epilepticus, alcohol withdrawal, preoperative sedation.
- Adverse Effects: Sedation, anterograde amnesia, impaired motor coordination, risk of falls, paradoxical agitation, dependence, withdrawal (potentially life-threatening seizures), respiratory depression (especially with other CNS depressants).
- Special Populations:
- Elderly: Increased sensitivity, risk of falls, cognitive impairment.
- Pregnancy: Teratogenicity and neonatal withdrawal (avoid especially in first trimester).
II. Barbiturates (Historic/rare)
- Drugs: Phenobarbital, secobarbital
- Role: Once major anxiolytic/sedative agents; now replaced by benzodiazepines due to high toxicity, overdose risk, induction of hepatic enzymes, and physical dependence.
III. SSRIs and SNRIs
- Major Drugs: Paroxetine, Sertraline, Escitalopram, Fluoxetine (SSRIs); Venlafaxine, Duloxetine (SNRIs)
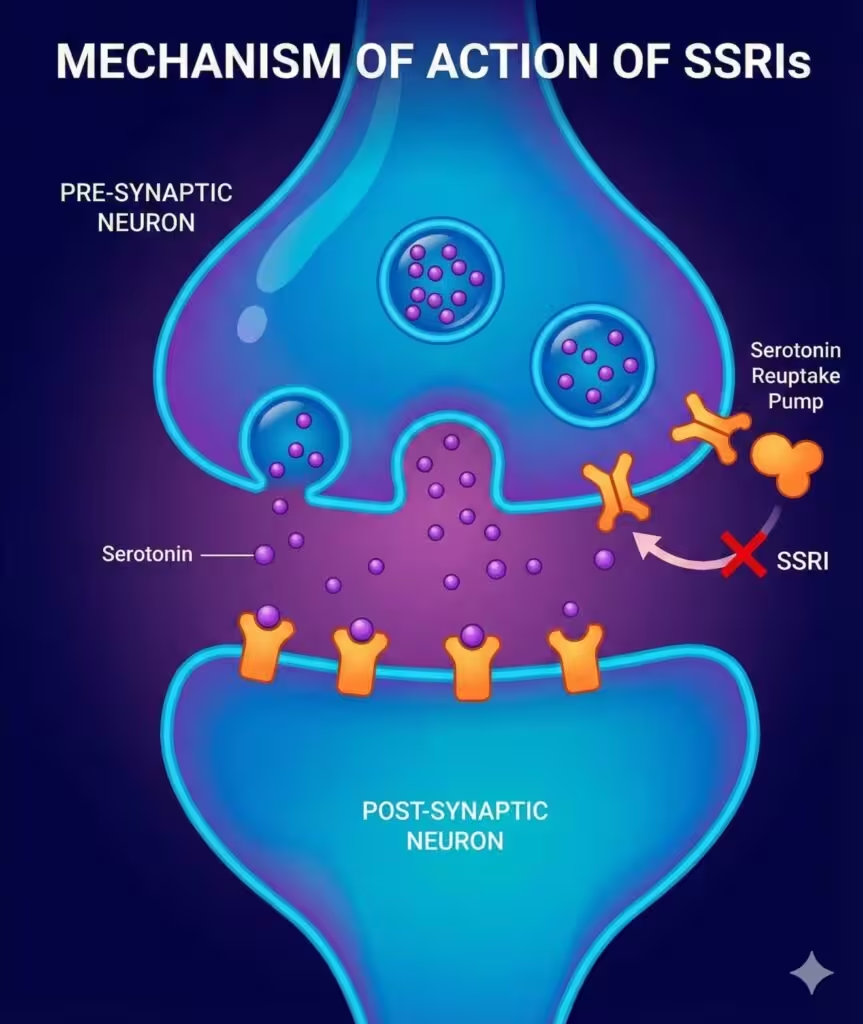
- Mechanism: Inhibit reuptake of serotonin (SSRIs) and serotonin/noradrenaline (SNRIs) into presynaptic neurons. This potentiates serotonergic neurotransmission in CNS limbic regions implicated in mood and anxiety.
- Pharmacokinetics:
- Absorption: Well absorbed orally; variable protein binding.
- Metabolism: Hepatic CYP enzymes; some have active metabolites (fluoxetine/norfluoxetine).
- Elimination half-life: Long (fluoxetine: up to 7 days for metabolite).
- Clinical Use: Chronic management of anxiety disorders (GAD, OCD, panic disorder, PTSD).
- Adverse Effects: GI symptoms, sexual dysfunction, sleep disturbance, initial anxiety aggravation (dose titrate), weight changes, rare: hyponatremia, serotonin syndrome (especially with MAOIs).
- Special Points: No risk of dependence; withdrawal symptoms can occur if abruptly discontinued.
IV. Buspirone
- Mechanism: Partial agonist at 5-HT1A1A receptor; minor affinity for D22 receptors. Reduces presynaptic firing, modulates serotoninergic pathways.
- Pharmacokinetics: Well absorbed, hepatic CYP3A4 metabolism, short half-life (2–8 h). No active metabolites.
- Clinical Use: Generalized anxiety disorder; less effective for panic, not useful in severe acute anxiety.
- Adverse Effects: Dizziness, headache, minimal sedation, no dependence/withdrawal.
- Onset: Delayed (1–2 weeks for effect); not for acute anxiety relief.
V. Antihistamines (Sedating H11 blockers)
- Major Drugs: Hydroxyzine, Diphenhydramine
- Mechanism: Competitive antagonist of central/peripheral H11 receptors; some anticholinergic activity.
- Clinical Use: Short-term anxiety, preoperative sedation, adjunct for insomnia.
- Adverse Effects: Sedation, anticholinergic symptoms (dry mouth, urinary retention, constipation), rarely cardiac arrhythmias (QT prolongation).
VI. Beta-Adrenergic Antagonists
- Major Drug: Propranolol
- Mechanism: Competitive inhibitor of peripheral beta-adrenergic receptors; blocks autonomic manifestations (tachycardia, tremor).
- Clinical Use: Performance/social/situational anxiety (stage fright); useful in conjunction with other anxiolytics.
- Adverse Effects: Bradycardia, hypotension, bronchospasm (avoid in asthma), fatigue, depression.
VII. Other Agents
- Pregabalin/Gabapentin: Decrease presynaptic calcium influx via α2δ subunits—reduce neurotransmitter release. Used in GAD, especially where comorbid neuropathy present.
- Etifoxine: Increases neurosteroid production, modulates GABAAA; approved in some countries for anxiety.
Comprehensive Table: Anxiolytics Properties and Use
| Class | Drug | Mechanism | Indications | Onset | Dependence Risk | Major AEs | Special Notes |
|---|---|---|---|---|---|---|---|
| Benzodiazepine | Diazepam | GABAA ↑ | Acute panic, withdrawal, muscle spasm | Minutes | High | Sedation, withdrawal | Active metabolites |
| Benzodiazepine | Lorazepam | GABAA ↑ | Acute, elderly, hepatic impairment | Minutes | High | Sedation, amnesia | No active metabolites |
| SSRI | Sertraline | 5-HT reuptake ↓ | GAD, panic, OCD, PTSD | Weeks | None | GI, sexual, anxiety | Start low, titrate |
| SNRI | Venlafaxine | 5-HT/NE reuptake ↓ | GAD, panic, social anxiety | Weeks | None | GI, hypertension | Monitor BP, withdrawal |
| Buspirone | Buspirone | 5-HT1A partial ↑ | GAD, chronic use | Weeks | None | Dizziness, headache | No sedation/dependence |
| Antihistamine | Hydroxyzine | H1 block | Short-term anxiety, insomnia | Minutes | None | Sedation, anticholin. | Limited for chronic use |
| Beta-blocker | Propranolol | β block | Situational anxiety | Minutes | None | Fatigue, bradycardia | Avoid in asthma |
| Other | Pregabalin | Ca2+ channels ↓ | GAD with pain | Minutes | Mild | Sedation, dizziness | Neuropathic pain |
Clinical Application and Prescribing Principles
Diagnosis Matching:
- GAD: SSRIs, SNRIs, buspirone. Benzodiazepines as short-term adjunct.
- Panic disorder: SSRIs/SNRIs mainstay; benzodiazepines for severe episodes.
- Social/performance anxiety: SSRIs/SNRIs, propranolol for performance situations.
- OCD/PTSD: SSRIs/SNRIs preferred.
Prescribing Strategy:
- Start low, titrate slow—especially for SSRIs/SNRIs to avoid initial agitation.
- Use benzodiazepines short-term (max 2–4 weeks) due to dependence risk. Avoid in patients with substance use history.
- Monitor for withdrawal symptoms: with benzodiazepines, SSRIs/SNRIs.
- Integrate with CBT/psychotherapy; medications augment therapy, especially for severe or persistent symptoms.
Adverse Effect Details and Drug Interactions
Benzodiazepines
- Tolerance develops for sedation; anxiolytic effects persist longer
- Interactions: Potentiated by other CNS depressants (alcohol, opioids), CYP3A4 inhibitors (ketoconazole, erythromycin increase benzodiazepine blood levels).
- Withdrawal: Abrupt cessation risky—taper gradually over weeks/months.
SSRIs/SNRIs
- Sexual dysfunction is common—may require switch or adjunctive therapy.
- Serotonin syndrome: Risk increased with MAOIs, St John’s Wort, other serotonergic drugs.
- Discontinuation syndrome: Dizziness, insomnia, flu-like symptoms after abrupt stop—taper over weeks.
Buspirone
- No sedation/respiratory depression.
- CYP3A4 inhibitors: Increase buspirone levels; dose adjust.
Antihistamines and Beta-blockers
- Anticholinergic burden: Watch for delirium risk in elderly.
- Beta-blockers: Additive effect with other hypotensive agents.
Special Considerations by Population
Elderly
- Prefer SSRIs/SNRIs or buspirone to avoid sedation and fall risk.
- Benzodiazepines only if no other option, at lowest effective dose.
Pregnancy
- SSRIs safest but still require risk:benefit analysis.
- Benzodiazepines generally contraindicated (risk of orofacial clefts, neonatal withdrawal, respiratory depression).
Children
- SSRIs mainstay where indicated; use benzodiazepines with extreme caution—risk for behavioral/cognitive disturbances.
Non-Pharmacological and Combined Management
- CBT and behavioral therapies demonstrated efficacy equal or superior to medication in mild-moderate anxiety.
- Lifestyle modifications: Physical activity, mindfulness/meditation, regular sleep, avoidance of stimulants (caffeine, nicotine).
- Integration: Severe symptoms may require combined pharmacotherapy and psychotherapy.
- Monitoring: Regular review for efficacy, adverse effects, and need for dose adjustment or switching.
Emerging Anxiolytics and Research
- Novel GABAAA modulators: Subtype-selective (e.g., α2/α3-targeting agents) for anxiolysis without sedation/dependence.
- Neuroactive steroids: Allopregnanolone analogs in late-phase clinical trials—modulate GABAAA distinctly from benzodiazepines.
- Cannabinoids (CBD): Promising for mild anxiety—unclear regulation and clinical utility.
- Digital/Neuromodulation therapies: rTMS, VR-augmented CBT, app-based interventions.
Summary Table – Key Facts
| Key Point | Evidence Highlight |
|---|---|
| Benzodiazepines: rapid, short-term relief | High dependence risk—recommend <4 weeks only |
| SSRIs/SNRIs: first-line for chronic anxiety | Non-sedating, slow onset, discontinuation effects |
| Buspirone: GAD only | Minimal sedation, delayed onset |
| Hydroxyzine/antihistamines: short-term use | Sedation, anticholinergic burden |
| Beta-blockers: physical symptoms only | Do not treat anxiety per se |
Conclusion
The pharmacological management of anxiety demands strategic selection of agents based on diagnosis, patient context, side effect profile, and risk of dependence. Benzodiazepines are reserved for acute crises; SSRIs/SNRIs and buspirone are backbone agents for chronic disorders. Safe prescribing requires careful titration, population-specific caution, and ongoing monitoring. Non-pharmacological interventions, especially CBT, should be integral to care. The future of anxiolytic therapy promises highly selective drugs, multimodal interventions, and personalized care pathways.
Detailed References for Clinical Authenticity
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition: Chapter Sedative-Hypnotic Drugs.
- Katzung BG, Basic & Clinical Pharmacology, 15th Edition: Chapter Sedative-Hypnotics and Anxiolytics.
- Rang HP, Dale MM, Rang & Dale’s Pharmacology, 8th Edition: “CNS Drugs,” Anxiety and Sleep.
- OpenStax Pharmacology: Section 13.4 Anxiolytics.
- Selected journal articles/review: PMC6340395, PMC3263390, PMC3482271, PMC4209938, ADA-4-129.
Anxiolytics and Lifestyle
The Importance of a Holistic Approach
While anxiolytics play a crucial role in managing anxiety, a holistic approach that includes lifestyle changes can significantly enhance treatment outcomes. This comprehensive method acknowledges that medication alone may not address all aspects of an anxiety disorder. Combining pharmacological treatments with lifestyle modifications can improve overall well-being, reduce dependency on medications, and potentially decrease the severity and frequency of anxiety symptoms.
Lifestyle Changes That Complement Anxiolytics
Regular Physical Activity
Exercise has been shown to reduce anxiety symptoms due to the release of endorphins, natural mood lifters. It also helps improve sleep and reduce stress.
Balanced Diet
Eating a healthy diet can impact mood and anxiety. Foods rich in omega-3 fatty acids, antioxidants, and vitamins can support brain health and reduce anxiety symptoms.
Mindfulness and Relaxation Techniques
Practices such as meditation, yoga, and deep-breathing exercises can decrease stress levels and enhance the effectiveness of anxiolytics by promoting relaxation of the mind and body.
Adequate Sleep
Poor sleep can exacerbate anxiety, while quality sleep can help reduce it. Establishing a regular sleep schedule and a calming bedtime routine can improve sleep quality.
Limiting Stimulants
Reducing or eliminating the intake of caffeine and other stimulants can help lower anxiety levels, as these substances can increase nervousness and interfere with sleep.
The Future of Anxiolytics
Research Trends
Current research in anxiolytic treatment is exploring various avenues, including the role of genetic factors in anxiety disorders, the potential for personalized medicine, and the development of drugs with fewer side effects and lower risks of dependency.
Potential New Treatments
One area of interest is the investigation of compounds that target novel neurotransmitter systems or those that offer a more targeted approach to modulating GABAergic activity. Additionally, there is growing interest in the therapeutic potential of CBD (cannabidiol) and other cannabinoids in treating anxiety, due to their purported anxiolytic effects without the psychoactive properties of THC.
Emerging therapies, such as neuromodulation techniques (e.g., transcranial magnetic stimulation) and digital interventions (e.g., virtual reality exposure therapy), are also being explored for their potential to treat anxiety disorders in conjunction with, or as an alternative to, traditional anxiolytics.
The future of anxiolytics lies in the development of treatments that are not only effective but also carry fewer risks and side effects. This, combined with a holistic approach that incorporates lifestyle changes, promises a more comprehensive and individualized strategy for managing anxiety.
Conclusion
Recap of Key Points
Throughout this exploration of anxiolytics and their role in anxiety management, we’ve delved into various aspects of these medications, including their types, mechanisms of action, and considerations for use in special populations. We’ve underscored the importance of GABA in the pharmacology of anxiety and how anxiolytics, particularly benzodiazepines and SSRIs, modulate this neurotransmitter system to alleviate symptoms of anxiety.
The discussion highlighted the necessity of adopting a holistic approach to anxiety management, emphasizing that while anxiolytics can be highly effective in reducing anxiety symptoms, lifestyle modifications—such as regular exercise, a balanced diet, mindfulness practices, adequate sleep, and limiting stimulants—play a crucial complementary role.
Looking ahead, we touched upon the promising future of anxiolytic treatment, spotlighting ongoing research into new pharmacological targets, the potential for personalized medicine based on genetic profiling, and the exploration of novel treatments, including cannabinoids and neuromodulation techniques.
Moving Forward with Anxiety Management
As we move forward, it’s clear that the management of anxiety disorders will continue to evolve, driven by advancements in neuroscience, pharmacology, and a deeper understanding of the bio-psycho-social factors contributing to anxiety. The shift towards more personalized and holistic treatment plans, incorporating both anxiolytics and lifestyle changes, is likely to provide more effective, sustainable, and patient-centered care.
For individuals living with anxiety, this means there is hope for more targeted and tolerable treatments with fewer side effects, alongside a greater emphasis on non-pharmacological interventions that empower individuals to manage their anxiety in a way that suits their unique needs and lifestyles.
In conclusion, the journey towards mastering anxiety is multifaceted, combining the science of medication with the art of lifestyle modifications. By continuing to advance our understanding and treatment approaches, we can look forward to a future where anxiety is not just manageable but where individuals can thrive, unfettered by the constraints of their symptoms.
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.