I. Introduction and Electrophysiological Basis
Cardiac arrhythmias are disorders of the heart rate or rhythm caused by abnormalities in electrical impulse formation or conduction. Antiarrhythmic drugs (AADs) aim to restore normal sinus rhythm (NSR) or control ventricular rate, though they are characterized by a narrow therapeutic index and a paradoxical potential to induce lethal arrhythmias (proarrhythmia).
To understand the pharmacodynamics of these agents, one must first master the cardiac action potential (AP).
A. The Cardiac Action Potential
Cardiac cells are broadly categorized into two electrical types:
- Fast-Response Fibers: (Atria, Ventricles, His-Purkinje system). Dependent on voltage-gated \(Na^+\) channels.
- Slow-Response Fibers: (Sinoatrial [SA] node, Atrioventricular [AV] node). Dependent on \(Ca^{2+}\) channels; exhibit automaticity.
Fast-Response Phases
- Phase 0 (Rapid Depolarization): Triggered when membrane potential (\(V_m\)) reaches threshold (-70 mV). Massive influx of \(Na^+\) via voltage-gated channels (\(I_{Na}\)). The maximum upstroke velocity (\(dV/dt_{max}\)) determines conduction velocity.
- Phase 1 (Early Repolarization): Rapid inactivation of \(Na^+\) channels and transient efflux of \(K^+\) via \(I_{to}\) (transient outward current).
- Phase 2 (Plateau): A balance between inward depolarizing \(Ca^{2+}\) currents (\(I_{Ca-L}\)) via L-type calcium channels and outward repolarizing \(K^+\) currents. This phase prolongs the refractory period, preventing tetany.
- Phase 3 (Repolarization): \(Ca^{2+}\) channels close. \(K^+\) efflux dominates via delayed rectifier currents: rapid (\(I_{Kr}\)) and slow (\(I_{Ks}\)). This returns \(V_m\) to resting levels.
- Phase 4 (Resting Potential): Maintained by the \(Na^+/K^+\)-ATPase pump and the inward rectifier current (\(I_{K1}\)), stabilizing \(V_m\) at approximately -85 to -90 mV.
Slow-Response Phases (Pacemaker Cells)
These cells lack a stable Phase 4.
- Phase 0: Slower upstroke mediated by \(Ca^{2+}\) entry (\(I_{Ca-L}\)), not \(Na^+\).
- Phase 3: Repolarization via \(K^+\) efflux.
- Phase 4 (Pacemaker Potential): Spontaneous diastolic depolarization caused by the “funny current” (\(I_f\)), a mixed \(Na^+/K^+\) inward current activated by hyperpolarization.
II. Mechanisms of Arrhythmia
Arrhythmias arise from three primary mechanisms. AADs work by targeting these specific anomalies.
1. Abnormal Automaticity
- Enhanced Normal Automaticity: Accelerated firing of the SA node or latent pacemakers due to sympathetic stimulation (\(\beta\)-adrenergic) or hypokalemia.
- Abnormal Automaticity: Cells that do not normally pace (e.g., ventricular myocytes) spontaneously depolarize due to ischemia or injury currents.
2. Triggered Activity
Oscillations in membrane potential that occur during or immediately after an AP.
- Early Afterdepolarizations (EADs): Occur during Phase 2 or 3. Associated with prolonged Action Potential Duration (APD). Clinical correlate: Torsades de Pointes (TdP).
- Delayed Afterdepolarizations (DADs): Occur during Phase 4. Caused by intracellular \(Ca^{2+}\) overload (e.g., Digoxin toxicity, catecholamine excess).
3. Re-entry
The most common mechanism for clinically significant arrhythmias (e.g., Atrial Fibrillation, VT). It requires:
- Two distinct pathways for impulse conduction.
- Unidirectional block in one pathway (often due to heterogeneity in refractoriness).
- Slowed conduction in the other pathway, allowing the blocked path to recover.
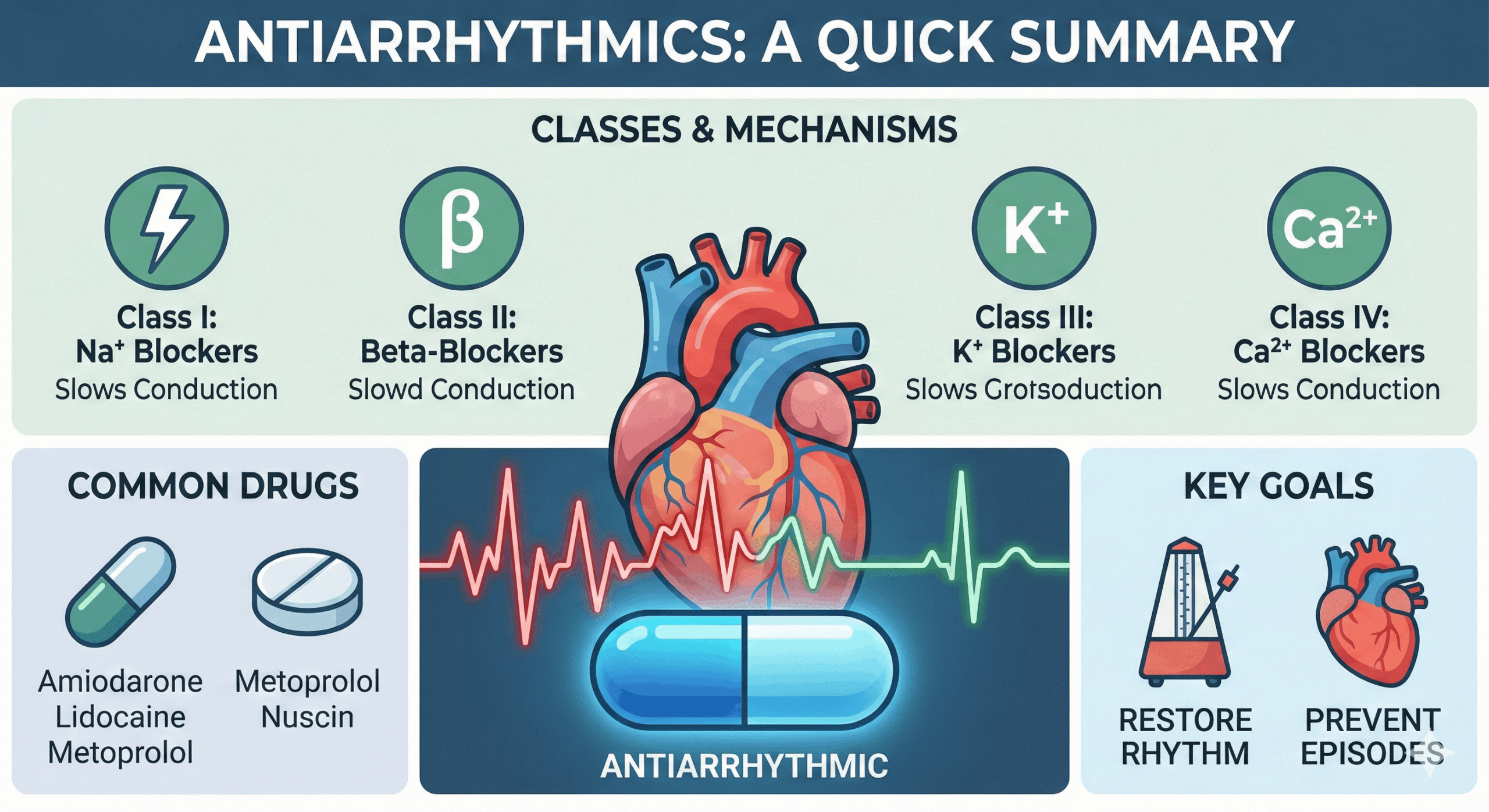
III. Classification of Antiarrhythmic Drugs
The Vaughan Williams (VW) classification, though imperfect, remains the clinical standard. It categorizes drugs based on their primary channel-blocking effect.
| Class | Primary Mechanism | Effect on AP | Primary Drugs |
|---|---|---|---|
| I | \(Na^+\) Channel Blockade | \(\downarrow\) Phase 0 Upstroke | (See Subclasses) |
| II | \(\beta\)-Adrenergic Blockade | \(\downarrow\) Phase 4 slope, \(\downarrow\) AV conduction | Metoprolol, Esmolol |
| III | \(K^+\) Channel Blockade | \(\uparrow\) AP Duration (Phase 3) | Amiodarone, Sotalol, Dofetilide |
| IV | \(Ca^{2+}\) Channel Blockade | \(\downarrow\) AV conduction | Verapamil, Diltiazem |
| Misc | Adenosine / Pump inhibition | Various | Adenosine, Digoxin |
IV. Class I: Sodium Channel Blockers
Class I agents block the fast inward sodium current (\(I_{Na}\)). Their binding is state-dependent, meaning they bind more avidly to open or inactivated channels than to resting channels. This leads to Use-Dependence: the drug effect is more pronounced at faster heart rates.
Class Ia: Intermediate Kinetics
- Drugs: Quinidine, Procainamide, Disopyramide.
- Mechanism: Moderate blockade of \(I_{Na}\) and blockade of \(I_K\).
- Effects: Slows Phase 0; Prolongs APD and ERP (due to \(I_K\) block). ECG shows widened QRS and prolonged QT.
- Clinical Pearls:
- Quinidine: “Cinchonism” (tinnitus, headache), GI distress. Potent CYP2D6/P-gp inhibitor.
- Procainamide: Chronic use causes Drug-Induced Lupus Erythematosus (DILE).
- Disopyramide: Strong anticholinergic effects; negative inotrope (avoid in HF).
Class Ib: Fast Kinetics
- Drugs: Lidocaine, Mexiletine.
- Mechanism: Weak blockade of \(I_{Na}\); binds preferentially to inactivated channels.
- Effects: Minimal effect on Phase 0 in normal tissue; shortens APD. Selective for ischemic tissue.
- Clinical Pearls:
- Indications: Ventricular arrhythmias only (post-MI). Ineffective for atrial arrhythmias.
- Lidocaine: CNS toxicity is dose-limiting (confusion, seizures). High first-pass metabolism.
Class Ic: Slow Kinetics
- Drugs: Flecainide, Propafenone.
- Mechanism: Potent blockade of \(I_{Na}\). Extremely slow dissociation.
- Effects: Marked slowing of Phase 0; No effect on APD. Marked QRS widening.
- Clinical Pearls:
- Pill-in-the-Pocket: For paroxysmal AFib in structurally normal hearts.
- CAST Trial Warning: Increased mortality in post-MI patients. Contraindicated in structural heart disease.
V. Class II: Beta-Adrenergic Antagonists
Drugs: Metoprolol, Atenolol, Propranolol, Esmolol.
Mechanism: Competitive blockade of \(\beta_1\) receptors. Decreases cAMP and PKA activity, reducing phosphorylation of L-type \(Ca^{2+}\) and \(I_f\) channels.
Effects: Decreases Phase 4 slope in SA node (\(\downarrow\) HR); Decreases conduction velocity in AV node (\(\uparrow\) PR interval).
VI. Class III: Potassium Channel Blockers
These agents prolong the Action Potential Duration (APD) and Effective Refractory Period (ERP) by blocking potassium repolarizing currents (primarily \(I_{Kr}\)).
Amiodarone
The dominant antiarrhythmic in clinical practice.
- Mechanism: “Broad Spectrum” (Classes I, II, III, and IV activity).
- Pharmacokinetics: Huge Volume of Distribution (\(V_d \approx 60 L/kg\)). Half-life 26–100 days.
- Adverse Effects: Pulmonary fibrosis (monitor CXR), Thyroid dysfunction (contains iodine), Hepatic toxicity, Corneal microdeposits, Blue-gray skin.
- Interactions: Inhibits CYP3A4, CYP2C9, P-gp. Increases Warfarin/Digoxin levels.
Sotalol
Racemic mixture. L-isomer is a \(\beta\)-blocker; both D- and L-isomers block \(I_{Kr}\). Exhibits Reverse Use-Dependence (more effective at slow heart rates), increasing TdP risk during bradycardia.
VII. Class IV: Calcium Channel Blockers (Non-DHPs)
Drugs: Verapamil, Diltiazem.
Mechanism: Block \(L\)-type \(Ca^{2+}\) channels in Slow Response tissues (SA/AV nodes).
Indications: PSVT termination, Rate control in AFib.
VIII. Miscellaneous Agents
Adenosine
Mechanism: Activates \(A_1\) receptors in AV node \(\to\) activates \(I_{K-Ado}\) \(\to\) hyperpolarization.
Clinical Use: The “Chemical Reset Button” for PSVT. Very short half-life (<10s).
Digoxin
Mechanism: Inhibits \(Na^+/K^+\)-ATPase \(\to\) \(\uparrow\) intracellular \(Ca^{2+}\) (inotropy). Indirectly increases vagal tone to slow AV conduction.
Magnesium Sulfate
Use: Drug of choice for Torsades de Pointes, regardless of serum Mg levels.
IX. Summary: Channel Effects
| Drug Class | \(Na^+\) Block | \(K^+\) Block | \(Ca^{2+}\) Block | \(\beta\) Block | Clinical Context |
|---|---|---|---|---|---|
| Ia | ++ (Open) | ++ | – | – | AFib, WPW. Risk of TdP. |
| Ib | + (Inact.) | – | – | – | VT (Post-MI). CNS toxicity. |
| Ic | +++ (Open) | – | – | +/- | AFib (Healthy heart). Contra in CAD. |
| III | + (Amio) | +++ | + (Amio) | + (Amio) | AFib/VT. Amio safe in HF. |
| IV | – | – | +++ | – | SVT, Rate control. Avoid in HFrEF. |
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.