Class III antiarrhythmics predominantly prolong cardiac repolarization via potassium channel blockade, with amiodarone as the prototypical agent and additional options including dofetilide, sotalol, ibutilide, and dronedarone chosen based on structural heart disease, heart failure status, and proarrhythmic risk.
These drugs extend action potential duration and the QT interval to prevent reentry, while differing substantially in extracardiac toxicity, need for in‑hospital initiation, and suitability in heart failure, which is reflected in contemporary ACC/AHA/HRS and ESC guideline algorithms.
Class definition
Class III agents inhibit repolarizing potassium currents (notably IKrIKr), increasing effective refractory period and prolonging the QT interval, thereby suppressing reentrant circuits in atrial and ventricular myocardium.
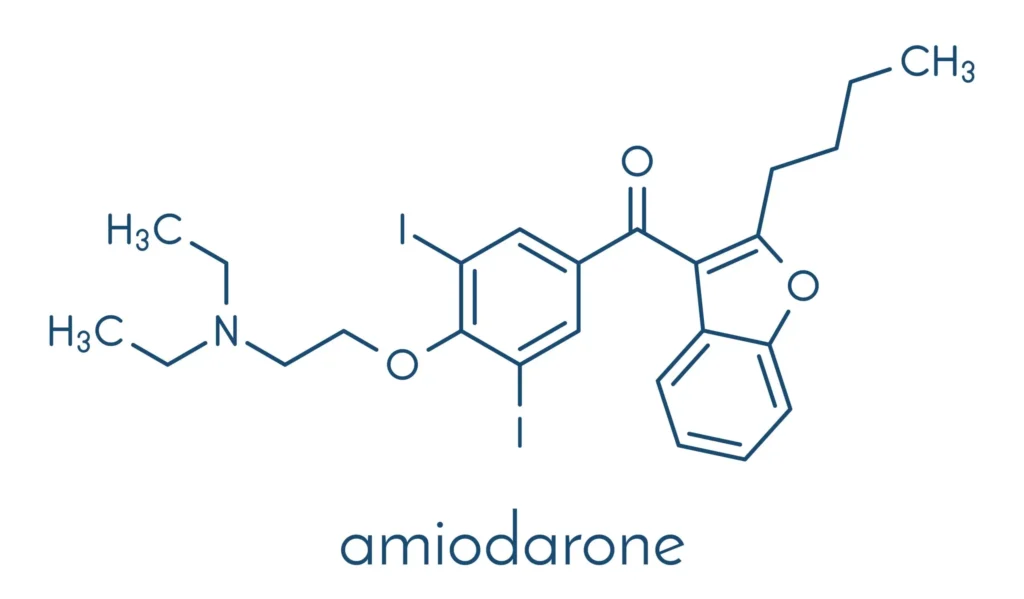
Amiodarone is pharmacologically pleiotropic (blocking K++, Na++, Ca2+ channels and exhibiting antiadrenergic effects), while dofetilide is a relatively selective IKrIKr blocker, sotalol combines nonselective beta‑blockade with IKrIKr inhibition, and ibutilide is administered IV for acute conversion with strong torsades monitoring requirements.
Electrophysiology
By prolonging phase 3 repolarization, Class III drugs lengthen action potential duration and refractoriness, which manifests as QTc prolongation on ECG and a variable risk of torsades de pointes across agents.
Amiodarone paradoxically carries a relatively low torsades risk compared with dofetilide and sotalol despite QT prolongation, whereas ibutilide has a well‑recognized acute torsades risk during and shortly after infusion requiring continuous ECG monitoring.
Amiodarone
- Indications: Labeled for life‑threatening ventricular tachycardia/fibrillation and widely used for atrial fibrillation/flutter when other options are unsuitable or in heart failure due to its minimal negative inotropy in HFrEF contexts.
- Pharmacology: Multichannel blocker (Class I/II/III/IV actions) with an exceptionally long half‑life 15–14215–142 days, leading to prolonged persistence of effects and drug–drug interactions after discontinuation.
- Adverse effects: Pulmonary toxicity, thyroid dysfunction (hypo/hyperthyroidism from iodine content), hepatic injury, corneal microdeposits, photosensitivity, and neuropathy necessitate baseline and periodic organ surveillance.
- Interactions: Numerous CYP- and P‑gp–mediated interactions (e.g., with warfarin and digoxin) and additive bradycardia/QT effects warrant careful medication reconciliation and INR/digoxin monitoring when initiated or adjusted.
Dofetilide
- Role: Oral, relatively selective IKrIKr blocker indicated for conversion and maintenance of sinus rhythm in symptomatic atrial fibrillation/flutter, with neutral mortality in high‑risk cohorts in DIAMOND and related evidence summaries.
- Initiation: Must be started in hospital with serial QTc monitoring and creatinine clearance–based dosing due to torsades risk; ongoing monitoring and avoidance of interacting QT‑prolonging drugs are required.
- Safety: Torsades de pointes risk rises with QTc prolongation and overdose; management parallels standard TdP care with IV magnesium and overdrive pacing if needed.
Sotalol
- Role: Nonselective beta blocker plus IKrIKr blockade for maintenance of sinus rhythm in AF/AFl and for ventricular arrhythmias, with a boxed warning for life‑threatening proarrhythmia.
- Initiation: Commonly requires inpatient initiation (traditionally ≥3 days) with renal function–guided dosing and serial QTc checks; an IV loading pathway exists to streamline transition to oral dosing under continuous telemetry.
- Safety: Torsades risk increases with QTc prolongation, hypokalemia/hypomagnesemia, and renal impairment, necessitating electrolyte optimization and dose adjustments.
Ibutilide
- Role: Intravenous agent for acute chemical cardioversion of atrial flutter and atrial fibrillation, with higher efficacy in typical flutter and rapid onset of action.
- Dosing/monitoring: Typical dosing is 11 mg IV over 1010 minutes if weight ≥60≥60 kg (or 0.010.01 mg/kg if <60<60 kg), repeatable once, with continuous ECG and at least 44 hours of post‑infusion telemetry and pre‑treatment correction of K/Mg to mitigate torsades risk.
- Safety: Marked proarrhythmic potential mandates monitoring until QTc normalizes and avoidance in pronounced baseline QT prolongation or severe LV dysfunction.
Dronedarone
- Profile: A non‑iodinated amiodarone analogue for AF in patients in sinus rhythm to reduce hospitalization, with multichannel and antiadrenergic effects but less thyroid/pulmonary toxicity than amiodarone.
- Contraindications: Harm in heart failure with recent decompensation or NYHA class IV and in permanent AF led to strict restrictions and contraindications by regulators and guidelines (informed by ANDROMEDA and PALLAS).
- Use case: Consider for maintenance in selected patients without advanced heart failure or permanent AF when amiodarone is undesirable, understanding its modest QT effect and interaction profile.
Guideline placement
The 2023 ACC/AHA/ACCP/HRS AF guideline recommends selecting antiarrhythmics by structural heart disease and HF status: in patients without prior MI or significant structural disease, dofetilide, dronedarone, flecainide, propafenone are Class IIa options and sotalol is IIb, with amiodarone also IIa but generally reserved for when others are unsuitable.
With prior MI or significant structural heart disease (including HFrEF), flecainide and propafenone are harmful, whereas amiodarone and dofetilide are IIa options and sotalol is IIb, while dronedarone is harmful in recent decompensated or advanced heart failure.
Torsades risk
Torsades de pointes risk is highest with potent QT‑prolonging pure IKrIKr blockers (e.g., dofetilide) and with sotalol, necessitating inpatient initiation and strict QTc/electrolyte protocols, while amiodarone’s torsades risk is comparatively low despite QT prolongation.
For ibutilide, continuous monitoring during infusion and for at least 44 hours post‑dose with pre‑treatment magnesium and potassium repletion is standard to reduce early afterdepolarizations and torsades events.
Heart failure context
In HFrEF, amiodarone and dofetilide are generally preferred for rhythm control based on safety data and guideline designation, while dronedarone is contraindicated in recent decompensation or NYHA IV and sotalol must be used cautiously with attention to QT and renal function.
This stratification aligns with neutral mortality data for dofetilide in advanced HF (e.g., DIAMOND) and safety alerts for dronedarone in permanent AF and decompensated HF.
Monitoring
Before initiation and during up‑titration, obtain baseline ECG and repeat QTc after dosing adjustments, correct hypokalemia and hypomagnesemia, and apply renal dosing for dofetilide and sotalol, typically in monitored inpatient settings for initiation.
For amiodarone, implement baseline and periodic thyroid, hepatic, pulmonary, and ophthalmic surveillance due to cumulative toxicity and very long elimination half‑life that sustains adverse effects after discontinuation.
Drug interactions
Amiodarone has extensive CYP and P‑gp interactions (notably with warfarin and digoxin) and additive effects with other QT‑prolonging or bradycardic agents, requiring dose adjustments and closer INR/digoxin level monitoring.
Dofetilide and sotalol have numerous contraindicated co‑medications that increase QT or block renal cation transport, and both require avoidance of concurrent QT‑prolonging antiarrhythmics or macrolides/fluoroquinolones when possible.
Practical selection
- No structural heart disease: Consider dofetilide or dronedarone for maintenance, with sotalol as a secondary option and amiodarone generally reserved because of systemic toxicities.
- Structural disease/HFrEF: Prefer amiodarone or dofetilide for maintenance; avoid dronedarone in recent decompensation/NYHA IV; use sotalol cautiously with renal/QT protocols if chosen.
- Acute conversion: Use ibutilide under telemetry for recent‑onset AF/AFl (especially typical flutter) or consider electrical cardioversion per guideline strategy and availability.
Agent pearls
- Amiodarone: Broad efficacy across atrial and ventricular arrhythmias with low torsades risk but high extracardiac toxicity and a half‑life measured in weeks to months necessitating long‑term surveillance and careful interactions management.
- Dofetilide: Effective atrial antiarrhythmic with mandated inpatient start, strict QT/renal dosing protocol, and demonstrated rhythm‑maintenance benefits without mortality penalty in high‑risk cohorts.
- Sotalol: Dual beta‑blocker/Class III properties requiring inpatient initiation and renal dose adjustment, with torsades risk tied to QTc and kidney function.
- Ibutilide: Rapid IV cardioversion agent for AF/AFl with higher efficacy in flutter and stringent telemetry and electrolyte protocols to mitigate torsades.
- Dronedarone: Non‑iodinated amiodarone derivative for AF maintenance in selected patients, contraindicated in permanent AF and recent decompensated/advanced HF based on safety trials and regulatory guidance.
Key takeaways
Class III antiarrhythmics—especially amiodarone, dofetilide, sotalol, ibutilide, and dronedarone—prolong repolarization and are deployed according to structural heart disease and heart failure status to balance rhythm‑control efficacy with torsades and organ toxicity risks.
Guidelines prioritize dofetilide or amiodarone in HFrEF, allow dronedarone or dofetilide in structurally normal hearts, require inpatient initiation for dofetilide and sotalol, and emphasize rigorous QT/electrolyte monitoring and organ surveillance when using Class III therapies.
Quiz on antiarrhythmic drugs: class 3
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.

