Introduction
Loratadine is a widely used second-generation antihistamine renowned for its effectiveness in alleviating allergy symptoms such as sneezing, runny nose, and itchy or watery eyes. By selectively blocking peripheral histamine H₁-receptors, loratadine significantly diminishes the effects of endogenous histamine, thus relieving the hallmark symptoms of allergic rhinitis, urticaria, and other hypersensitivity ailments. Thanks to its preferential targeting of peripheral H₁ receptors, loratadine achieves potent antihistamine activity with minimal sedation—a marked improvement over older first-generation antihistamines such as diphenhydramine or chlorpheniramine.
Even decades after its introduction, loratadine remains a cornerstone medication for allergic conditions worldwide. Its success is partly due to its favorable safety profile, once-daily dosing, over-the-counter availability, and minimal risk of anticholinergic effects. This article presents a comprehensive discussion on the pharmacology of loratadine, sketching out its historical framework, chemical structure, mechanism of action, pharmacokinetic attributes, therapeutic applications, adverse effect considerations, and future prospects. References in this article draw upon the 15th Edition of “Katzung BG, Basic & Clinical Pharmacology,” alongside other classic pharmacological resources including “Goodman & Gilman’s The Pharmacological Basis of Therapeutics” (13th Edition) and “Rang & Dale’s Pharmacology” (8th Edition).
Historical Background
Loratadine emerged in the late 1980s as an alternative to first-generation antihistamines that often induced sedation and anticholinergic side effects. The quest to discover second-generation antihistamines focused on designing molecules incapable of crossing the blood-brain barrier (BBB) readily, hence minimizing CNS depression. This structural ingenuity led to the creation of loratadine, introduced globally in the early 1990s.
Thanks to numerous clinical trials, loratadine soon garnered widespread acceptance, finding a prominent place among non-sedating antihistamines. Over time, post-marketing research reaffirmed its efficacy and comparatively benign side effect profile, facilitating conversion from prescription-only to over-the-counter (OTC) status in many countries. Today, loratadine competes alongside other second-generation agents like cetirizine and fexofenadine, yet continues to be widely prescribed and recommended by both pharmacists and physicians for allergic rhinitis and related conditions.
Chemical Structure
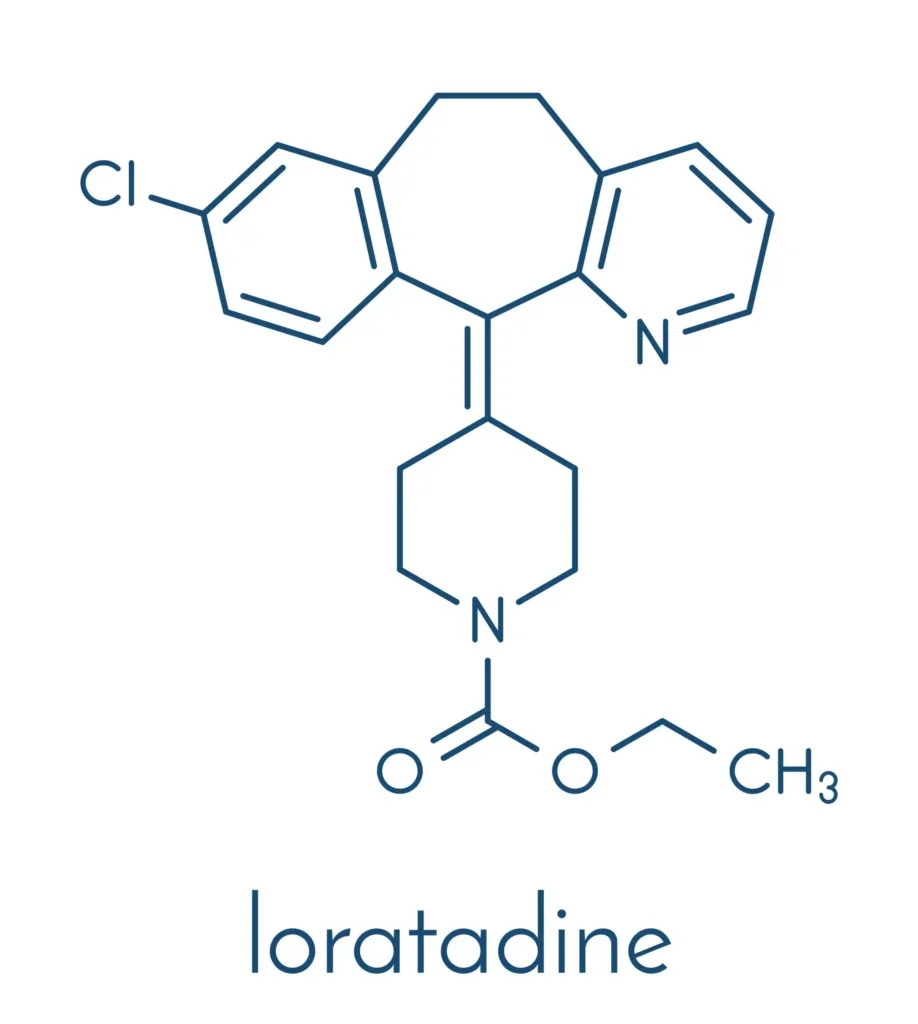
Loratadine is categorized as a tricyclic antihistamine, structurally related to drugs such as azatadine. Its chemical name is often reported as ethyl 4-(8-chloro-5,6-dihydro-11H-benzo[5,6]cyclohepta[1,2-b]pyridin-11-ylidene)-1-piperidinecarboxylate. The molecular framework is designed to be lipophilic enough to ensure efficient absorption but also configured in such a way to curtail central nervous system penetration.Key structural attributes:
- Tricyclic core reminiscent of older antihistamines yet modified with substituents that reduce BBB permeability.
- Chlorine substituent that modestly enhances binding to peripheral H₁ receptors.
- Carboxylate extension conferring partial ionic character, further restricting excess CNS access.
These chemical modifications partly explain loratadine’s “peripherally selective” behavior—a feature central to its low risk of sedation.
Mechanism of Action
Histamine H₁-Receptor Antagonism
Histamine, predominantly released by mast cells and basophils, provokes classical allergy symptoms via its action on H₁ receptors in the smooth muscle, endothelial cells, and nervous system. Allergic manifestations include vasodilation, increased vascular permeability (causing edema), itch, and bronchoconstriction. By competitively blocking these H₁ receptors, loratadine prevents histamine from exerting its effect, leading to a decrease in:
- Vasodilation and resultant nasal congestion or redness
- Vascular permeability, reducing edema formation
- Itch sensation, especially prominent in urticarial rashes and allergic rhinitis
Peripheral Selectivity
Second-generation antihistamines, including loratadine, have negligible affinity for muscarinic receptors and limited penetration of the BBB at recommended therapeutic doses. This characteristic generally spares the patient from the excessive sedation and anticholinergic side effects typical of earlier antihistamines. However, at very high dosages or in individuals with compromised BBB, a small fraction of loratadine and/or metabolites may enter the CNS, occasionally eliciting mild sedation.
Additional Activities
While loratadine is rarely described as having significant anti-inflammatory or immunomodulatory effects, ongoing research suggests that many modern antihistamines, including loratadine, might modestly reduce leukotriene and cytokine release or expression in allergy. Nonetheless, its principal utility remains predicated on H₁-receptor blockade.
Pharmacokinetics
Absorption
Loratadine is well absorbed via the gastrointestinal tract, with oral bioavailability ranging between 40% and 50%. This moderate bioavailability arises from presystemic metabolism in the liver (first-pass effect). Peak plasma concentrations typically appear in 1 to 2 hours when given orally. Ingredients in the formulation, such as lactose or other excipients, do not significantly alter absorption.
Distribution
Following absorption, loratadine circulates predominantly bound to plasma proteins (approximately 97–99%), keeping free drug levels relatively low. The drug’s lipophilic character leads to broad distribution throughout peripheral tissues. However, its structure largely impedes crossing of the BBB under normal circumstances—one reason sedation is uncommon at standard doses.
Metabolism
Loratadine undergoes extensive hepatic metabolism primarily via the cytochrome P450 system, notably CYP3A4 and CYP2D6. The chief metabolite is desloratadine, which also possesses potent H₁-receptor antagonistic activity and contributes significantly to the overall therapeutic effect.
- Desloratadine (active metabolite) has a considerably longer half-life, prolonging the efficacy window and permitting once-daily dosing.
- Phase II conjugation steps (glucuronidation, sulfation) may follow for further solubilization and excretion.
Excretion
Elimination transpires mainly via renal and fecal pathways as conjugated or unchanged metabolites. The plasma elimination half-life of loratadine is roughly 8 hours, while desloratadine can persist for up to 24–28 hours. This extended combined effect underscores the feasibility of once-daily dosing.
Special Considerations
- Hepatic Impairment: Diminished metabolic capacity can lead to higher plasma levels or prolonged action of loratadine and desloratadine.
- Renal Impairment: Alterations in excretory function may modulate drug half-lives.
- Elderly: Metabolism and elimination steps may be slower, advising possible dose adjustments or caution.
Overall, these pharmacokinetic nuances highlight loratadine’s convenience (daily dosing) and relative safety across varied patient populations when used prudently.
Clinical Indications and Uses
Allergic Rhinitis
Loratadine is widely prescribed or recommended for both seasonal (hay fever) and perennial allergic rhinitis. Commonly reported symptomatic relief includes decreased rhinorrhea, sneezing, nasal congestion, and ocular itching. With minimal sedation, it is well suited for daytime use.
Chronic Urticaria (Hives)
Clinical trials and broad clinical practice confirm loratadine’s efficacy for chronic idiopathic urticaria, alleviating itching and diminishing wheal formation. In many guidelines, second-generation antihistamines like loratadine are first-line therapy for mild to moderate urticarial conditions.
Other Allergic Dermatologic Conditions
For acute allergic skin reactions, drug rashes, or mild contact dermatitis, an H₁-blocker can reduce pruritus and associated inflammation. Although short-acting first-generation antihistamines can be advantageous at bedtime for sedation, second-generation agents like loratadine remain a popular choice for daytime symptom control.
Conjunctivitis
Allergic conjunctivitis—characterized by itchy, red, watery eyes—often accompanies rhinitis or occurs alone. Loratadine might mitigate ocular signs, though specialized antihistamine eye drops (e.g., olopatadine) frequently provide direct local relief.
Combination Use
Many OTC formulations marry loratadine with a decongestant such as pseudoephedrine to tackle nasal stuffiness more robustly. This synergy can be especially helpful in patients with prominent nasal congestion.
Dosage and Administration
Standard adult dosages for loratadine administration are usually 10 mg once daily for tablets, capsules, or orally disintegrating forms. Pediatric dosing depends on age and weight-based guidelines, but typically falls within 5 mg once daily for younger children (under 30 kg) or the adult dose for older/larger children.Administration Tips
- Typically taken orally with or without food
- Extended-release formulations (24-hour) are favored for consistent coverage
- Rapidly disintegrating or chewable tablets are beneficial for pediatric or geriatric populations who may face difficulty swallowing standard tablets
Patients commonly appreciate the once-daily regimen, ensuring compliance and persistent symptom coverage throughout the day.
Adverse Effects and Safety Profile
General Tolerability
Loratadine is generally well tolerated, and side effects—when present—are often mild. Headache, dry mouth, and fatigue represent the most frequently documented adverse events. However, these typically occur at low rates and are generally comparable to placebo in large clinical trials.
Sedation Potential
At therapeutic doses, sedation or drowsiness is uncommon because of limited loratadine penetration into the CNS. Nevertheless, a small minority of individuals may still experience mild sedation, particularly at higher-than-recommended doses or with concurrent use of CNS depressants.
Cardiac Safety
In contrast to some second-generation antihistamines (notably terfenadine or astemizole, withdrawn from many markets), loratadine exhibits minimal risk for QT prolongation at normal dosages. Serious cardiac arrhythmias (e.g., torsades de pointes) are quite rare for loratadine. However, caution may be warranted in patients with underlying heart conditions or concomitant use of potent CYP3A4 inhibitors that elevate plasma levels.
Hepatic and Renal Effects
No notable direct hepatotoxicity is typically associated with loratadine, though preexisting liver disease warrants prudent monitoring of any antihistamine therapy. Dose revision may be considered in severe hepatic or renal dysfunction to avoid drug/metabolite accumulation.
Hypersensitivity Reactions
Though rare, allergic or anaphylactic reactions to loratadine or excipients can occur. Symptoms may include rash, pruritus, or, in very rare instances, anaphylaxis.
Drug Interactions
CYP3A4 and CYP2D6 Inhibitors
Because loratadine is extensively metabolized by CYP3A4 and CYP2D6, potent inhibitors of these enzymes can amplify loratadine or desloratadine plasma concentrations. Examples encompass:
- Ketoconazole (potent CYP3A4 inhibitor)
- Itraconazole
- Erythromycin or Clarithromycin
- Certain protease inhibitors (e.g., ritonavir)
Prolonged, markedly raised drug levels could theoretically increase sedation risk or unmask rare cardiotoxicity, but clinically significant outcomes remain rare.
CNS Depressants
Though nominal in sedation, loratadine may potentiate mild sedation if combined with other CNS depressants (benzodiazepines, opioids, excessive alcohol). Caution is generally advised, though the synergy is less pronounced than with first-generation antihistamines.
Other Anticholinergic Agents
Loratadine itself poses minimal anticholinergic burden, so co-administration with anticholinergic medications is less worrisome compared to older antihistamines. Nonetheless, vigilance for increased dryness of mucous membranes or urinary retention is prudent in susceptible individuals.
Use in Special Populations
Pediatrics
Loratadine is frequently chosen for children with allergic rhinitis or mild urticaria because of its safety, ability to avoid sedation, and easy dosing forms (syrups, chewable tablets). Dosing must be approached carefully, conforming to established pediatric guidelines to avoid overdose or side effects.
Geriatrics
Older adults often benefit from loratadine because of its lower sedation and anticholinergic load, diminishing fall risks or cognitive impacts. However, age-related declines in hepatic/renal function prompt caution in dose adjustments if indicated.
Pregnancy and Lactation
Loratadine is generally classified under pregnancy risk category B or corridor, implying no well-known major risks in humans. It may be used if clearly needed, but as with any medication in pregnancy, risk-benefit deliberation is required. Because trace amounts can appear in breast milk, lactating mothers should consult healthcare professionals before use.
Hepatic Impairment
Diminished hepatic metabolism can prolong loratadine’s half-life. Clinical guidelines suggest lowering the daily dose (e.g., from 10 mg to 5 mg) or extending dosing intervals under moderate to severe liver dysfunction conditions.
Renal Impairment
Patients with significant renal insufficiency may excrete metabolites more slowly. Fulfillment of recommended dosing intervals or dosage reduction can help mitigate potential accumulation.
Advantages Over First-Generation Antihistamines
- Minimal Sedation: Minimal crossing of the BBB under usual doses keeps sedation low—beneficial for individuals requiring alertness (e.g., vehicle drivers, students).
- Less Anticholinergic Action: Reduced dryness of mouth, less urinary retention, and fewer vision problems than older agents (e.g., diphenhydramine, chlorpheniramine).
- Long Duration: Once-a-day dosing fosters adherence and consistent symptom relief.
- Better Tolerability: Fewer central side effects (like sedation or confusion), particularly valuable for older adults or those with comorbidities.
Comparison with Other Second-Generation Antihistamines
Cetirizine
- Cetirizine shares a potent H₁-blocking effect but can be more sedating than loratadine, presumably because it crosses the BBB more readily.
- While cetirizine is a strong anti-urticaria choice, individuals sensitive to drowsiness might prefer loratadine or fexofenadine.
Fexofenadine
- Fexofenadine (an active metabolite of terfenadine) demonstrates low sedation and lack of cardiotoxic potential.
- Clinically, loratadine and fexofenadine are considered comparable for allergic rhinitis. The choice may depend on patient response and tolerance.
Desloratadine
- This is the active metabolite of loratadine, featuring a longer half-life and potent H₁ receptor affinity. It’s functionally similar but can offer more extended coverage, used once daily in allergic rhinitis or urticaria.
Levocetirizine
- The R-enantiomer of cetirizine, credited with potent efficacy but a sedation tendency somewhat akin to cetirizine—albeit slightly improved sedation profile.
Patient Counseling Points
- Take Once Daily: Encourage compliance to reap continuous symptom control.
- Avoid Overuse: Exceeding recommended doses can inadvertently raise sedation risk or cause other side effects.
- Combination Decongestants: Some formulations contain pseudoephedrine; highlight potential side effects like insomnia or increased blood pressure.
- Alcohol: Remind patients that although sedation risks are small, combining with alcohol might intensify CNS depressant effects.
- Allergy Triggers: Emphasize the importance of identifying and minimizing exposure to allergens, as medication alone may not suffice for severe cases.
By setting realistic expectations and outlining how best to administer therapy, clinicians can optimize outcomes for patients taking loratadine.
Future Directions and Research
Extended Indications and Novel Combinations
Current trials investigate whether second-generation antihistamines like loratadine offer benefit in atopic dermatitis or chronic inflammatory conditions. Combined formulations with leukotriene receptor antagonists (e.g., montelukast) or intranasal corticosteroids hold potential for synergy in multi-symptom allergies.
Personalized Medicine
Polymorphisms in drug-metabolizing enzymes (CYP3A4, CYP2D6) can alter loratadine pharmacokinetics in certain individuals—raising prospects for genotype-driven dosage adjustments. Further research on such differences might refine personalized dosing and improve efficacy.
Topical or Inhaled Delivery
While loratadine is typically oral, future approaches might consider localizing therapy for targeted relief, for instance via nasal sprays. This might reduce systemic load while swiftly countering allergic rhinoconjunctivitis symptoms.
Pediatric and Geriatric Trials
Although widely used, data from large-scale, long-term clinical trials remains somewhat sparse, particularly in geriatric subpopulations with coexisting conditions. Further investigating safety and efficacy in these groups will help shape best practice recommendations.
Conclusion
Loratadine metamorphosed the management of allergy-related conditions with its novel blend of potent peripheral H₁-receptor antagonism and minimal CNS penetration, thus sparing patients from the drowsiness typical of first-generation antihistamines. Its once-daily dosing, wide therapeutic window, and strong safety profile reinforce its role as a mainstay in the pharmacotherapy of allergic rhinitis, urticaria, and affiliated allergic disorders.
Mechanistically, it operates by selectively inhibiting peripheral histamine receptors with minimal anticholinergic interference—resulting in fewer undesired effects at recommended dosages. Pharmacokinetically, loratadine enjoys good oral absorption, hepatic metabolism predominantly to active metabolite desloratadine, and excretion via renal and fecal routes, culminating in practical 24-hour symptom control. Clinically, it competes with other second-generation antihistamines like cetirizine and fexofenadine, but remains a top choice for patients seeking to minimize sedation.
Although it is generally well-tolerated, healthcare providers must remain attentive to the possibility of sedation at high doses, rare but potential drug interactions (e.g., with CYP3A4 inhibitors), or variable kinetics in hepatic/renal impairment. Through continued pharmacologic research and judicious clinical application, loratadine is likely to remain a flagship over-the-counter and prescription therapy for allergic conditions. The ongoing quest to refine combination products and novel delivery systems will further augment its utility in diverse patient populations around the world.
Citations
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- Katzung BG, Basic & Clinical Pharmacology, 15th Edition.
- Rang HP, Dale MM, Rang & Dale’s Pharmacology, 8th Edition.
📚 AI Pharma Quiz Generator
🎉 Quiz Results
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.

