If you trained in a time when every crash cart seemed to include “lido,” you remember lidocaine as the go-to antidote for ugly ventricular ectopy. Today, it has a more selective role—but when it is the right drug, it can be lifesaving. Lidocaine (also known as lignocaine) is a prototypical Class 1B antiarrhythmic with rapid kinetics, a strong preference for ischemic ventricular tissue, and a safety profile dominated by dose-related neurologic effects. This chapter walks through what clinicians and trainees need to know about lidocaine as an antiarrhythmic: how it works, where it fits, how to dose and monitor it, pitfalls, and pearls you can use immediately at the bedside.
Key takeaways:
- Class 1B sodium channel blocker with fast on–off kinetics, strong preference for inactivated channels in depolarized/ischemic ventricles, and minimal effects on normal atrial tissue and His–Purkinje conduction at therapeutic concentrations [1–3].
- Best established use: acute suppression of ventricular arrhythmias, especially in the context of myocardial ischemia or digitalis toxicity, and as an alternative when first-line agents (for example, amiodarone) fail or are unavailable in cardiac arrest due to pulseless VT/VF [1–3].
- IV only for antiarrhythmic use (extensive first-pass metabolism); short half-life with continuous infusion required; dose reductions needed in hepatic impairment, heart failure, shock, and in older adults [1–3].
- Dose-limiting toxicities are CNS effects (paresthesias, tremor, confusion, seizures). Serum levels can guide therapy if toxicity or inadequate response is suspected [1–3].
A QUICK ORIENTATION: WHAT MAKES CLASS 1B DIFFERENT
Class I antiarrhythmics block voltage-gated sodium channels, reducing excitability and conduction. Within Class I, lidocaine is 1B—fast binding and unbinding, strong preference for the inactivated channel state, and a tendency to shorten action potential duration (APD) in ventricular tissue [1–3].
What this means in practice:
- Selectivity for ischemic/depolarized tissue: Because ischemic myocytes tend to be partially depolarized with more sodium channels in the inactivated state, lidocaine binds preferentially where ectopy is most likely to arise—minimizing general conduction slowing [1–3].
- Little effect on atrial arrhythmias: Atria have shorter action potentials with fewer inactivated sodium channels at baseline; lidocaine’s affinity is lower there, so it’s generally ineffective for atrial tachyarrhythmias [1–3].
- Kinetics that favor tachycardia: Because binding and unbinding are very rapid, lidocaine exhibits “use dependence” mostly at higher rates in diseased tissue—further focusing its action where and when it’s most needed [1–3].
HOW LIDOCAINE WORKS: ELECTROPHYSIOLOGY WITHOUT THE JARGON
At the channel level
- Blocks fast sodium channels, favoring the inactivated state.
- Rapid association/dissociation (“fast on–off”) at physiologic pH.
- Reduces the slope of Phase 4 (automaticity) and slightly depresses Phase 0 upstroke in depolarized Purkinje/ventricular fibers; minimal effect on normal tissue at therapeutic levels [1–3].
At the tissue level
- Ventricular myocardium: Shortens APD and effective refractory period (ERP) slightly in Purkinje and ventricular fibers; the ERP/APD ratio can increase in diseased tissue, sometimes interrupting reentry [1–3].
- Ischemic preference: By stabilizing irritable, partially depolarized cells, lidocaine suppresses premature ventricular complexes and non-sustained and sustained ventricular tachycardia triggered in the ischemic substrate [1–3].
- His–Purkinje and AV nodal tissue: Minimal change at therapeutic concentrations, which helps avoid widespread conduction slowing [1–3].
ECG signatures
- Little to no change in PR or QRS at therapeutic levels in most patients.
- Action potential shortening can translate to a modest QT shortening, but QT changes are not a main clinical endpoint for lidocaine [2,3].
- Significant QRS widening or marked PR prolongation suggests excessive sodium channel blockade; re-evaluate dosing and serum level if present [2].
PHARMACOKINETICS: WHAT DETERMINES THE DOSE YOU CHOOSE
Formulations and route
- IV is the route for antiarrhythmic therapy. Oral bioavailability is low (extensive first-pass metabolism), making oral use impractical for acute arrhythmias [1–3].
- Many hospitals stock premixed bags (e.g., 1–2 g in 250 mL) and 2% lidocaine for boluses.
Distribution
- Rapid distribution from plasma to tissues; onset of antiarrhythmic effect within 45–90 seconds after IV bolus, peak within minutes [1–3].
- Large volume of distribution (~0.7–1.5 L/kg) due to lipophilicity; crosses the blood–brain barrier readily, explaining CNS effects at higher exposures [1–3].
- Protein binding ~60–80%, predominantly to alpha-1 acid glycoprotein (AAG). AAG levels rise in acute MI and critical illness, which can increase total plasma concentrations while decreasing free fraction; clinical effect correlates best with free (unbound) drug [1–3].
Metabolism and elimination
- Hepatic metabolism via CYP1A2 and CYP3A4 to active metabolites (monoethylglycinexylidide [MEGX] and glycinexylidide), which have less antiarrhythmic activity but contribute to CNS toxicity with accumulation [1–3].
- High hepatic extraction; clearance is flow-limited. Conditions that reduce hepatic blood flow (heart failure, shock) or inhibit CYP enzymes (e.g., cimetidine, certain beta blockers) decrease clearance [2,3].
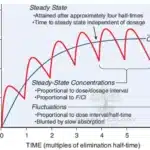
- Elimination half-life ~1.5–2 hours; extends to 3–4+ hours in liver dysfunction, heart failure, or with prolonged infusions (due to metabolite accumulation and saturation of distribution kinetics) [1–3].
- Renal impairment does not markedly change lidocaine clearance but can allow metabolite accumulation, increasing risk of neurologic adverse effects during prolonged infusions [1–3].
Dosing implications
- Use a weight-based IV bolus to rapidly fill the volume of distribution and achieve effect; follow with a continuous infusion titrated to response and tolerability [2,3].
- Reduce maintenance doses—and sometimes bolus—in older adults, hepatic disease, heart failure, shock, and after prolonged infusions [1–3].
CLINICAL INDICATIONS: WHERE LIDOCAINE STILL SHINES
1) Acute ventricular arrhythmias in ischemia
- Hemodynamically significant ventricular tachycardia (monomorphic or polymorphic) in the setting of acute ischemia or myocardial infarction, particularly when first-line therapies are contraindicated or ineffective [1–3].
- Frequent or multifocal PVCs or nonsustained VT with ischemia sometimes respond, though prophylactic suppression of benign ectopy post-MI does not improve outcomes and is not recommended [1–3].
2) Cardiac arrest due to VT/VF (alternative strategy)
- In refractory VT/VF arrest when standard measures (defibrillation, epinephrine) and preferred antiarrhythmic options are unsuccessful or unavailable, lidocaine remains a reasonable alternative. Contemporary practice often prioritizes amiodarone, but lidocaine is still taught and used in many systems as an alternative [1–3].
3) Digitalis-induced ventricular arrhythmias
- Historically, lidocaine (and phenytoin) has been recommended for digitalis-induced ventricular tachyarrhythmias; contemporary definitive therapy is digoxin-specific antibody fragments when toxicity is confirmed, but lidocaine is reasonable for acute arrhythmia suppression while definitive treatment is arranged [1–3].
4) Perioperative/postoperative ventricular arrhythmias
- Ventricular ectopy or VT in the perioperative setting, especially with myocardial irritability or ischemia, may respond to lidocaine. Its minimal hemodynamic depression is an advantage in hemodynamically fragile patients [1–3].
What lidocaine does not do well
- Atrial arrhythmias (AF/AFL/atrial tachycardia): Lidocaine has little effect on atrial tissue and is not recommended [1–3].
- Prophylactic suppression of PVCs post-MI: Although it reduces the incidence of VF, prophylactic use has not improved survival and may increase asystole; therefore not recommended [1–3].
HOW TO DOSE IT: A PRACTICAL BEDSIDE GUIDE
Initial IV bolus
- 1.0 to 1.5 mg/kg IV over 2–3 minutes (use actual body weight for loading; in morbid obesity, some clinicians cap at 100–120 mg per bolus while monitoring effect) [2,3].
- If VT/PVCs persist, repeat 0.5 to 0.75 mg/kg every 5–10 minutes to a maximum cumulative bolus dose of about 3 mg/kg in the first 30 minutes [2,3].
Continuous infusion
- Typical maintenance infusion: 1 to 4 mg/min (about 20–50 micrograms/kg/min), titrated to effect and tolerability [2,3].
- Reduce the infusion rate by 25–50% in:
- Older adults
- Hepatic impairment
- Heart failure or shock (reduced hepatic blood flow)
- After prolonged infusions (>24 hours), to minimize metabolite accumulation [1–3].
Endotracheal administration
- Historically described when IV/IO access is not available in arrest. Contemporary protocols de-emphasize this route due to variability in absorption. If used as a last resort, dose is higher than IV (often 2–3 times the IV bolus, diluted), but verify locally approved protocols [2,3].
Transitioning and duration
- Because the half-life is short, continuous infusion is needed to maintain suppression. Reassess the need for ongoing infusion frequently; many patients can be tapered when the ischemic trigger is corrected or a definitive strategy (revascularization, ablation, alternate antiarrhythmic) is implemented [1–3].
TARGET LEVELS AND MONITORING
Therapeutic range
- Commonly cited plasma concentration target: 1.5–5.0 micrograms/mL (total). Neurotoxicity often begins above 6 micrograms/mL, but clinical effect is better guided by patient response and signs of toxicity, especially when AAG binding changes total vs free levels [2,3].
When to check levels
- Suboptimal response after adequate loading and infusion.
- Signs of CNS toxicity (tremor, confusion, dysarthria, seizures).
- Prolonged infusions (>24–48 hours), particularly with renal impairment (metabolites) or hepatic dysfunction.
- Complex drug–drug interactions expected (e.g., strong CYP inhibitors) [2,3].
Bedside monitoring
- Continuous ECG and frequent vital signs.
- Watch for:
- Persistent or recurrent VT/PVCs despite adequate dosing.
- New or worsening conduction delay (especially marked QRS widening).
- CNS adverse effects: circumoral numbness, metallic taste, tinnitus, visual disturbances, agitation, confusion, tremor, myoclonus, seizures [1–3].
- Hemodynamic changes: hypotension or bradycardia are less common than with other sodium channel blockers but can occur at high doses or in compromised patients [2,3].
ADVERSE EFFECTS: WHAT TO EXPECT AND HOW TO MANAGE IT
Dose-related CNS effects
- Most common: lightheadedness, paresthesias (lips, tongue), dizziness, tinnitus, blurred vision, nausea, slurred speech, euphoria/dysphoria, tremor [1–3].
- At higher levels: confusion, agitation, hallucinations, myoclonus, seizures, coma, and respiratory depression [1–3].
- Management:
- Stop or reduce infusion; check serum level if available.
- Treat seizures with benzodiazepines; avoid large doses of propofol in unstable patients.
- Consider lipid emulsion therapy if features suggest severe local anesthetic systemic toxicity, particularly with very high exposures or inadvertent intra-arterial/intrathecal administration [2,3].
Cardiovascular effects
- Generally mild at therapeutic concentrations: minimal effects on myocardial contractility and systemic vascular resistance compared with Class 1C drugs.
- At toxic levels: hypotension, bradyarrhythmias, conduction disturbances, and rarely asystole [1–3].
- Management: reduce/stop infusion, supportive measures, atropine or pacing for significant bradyarrhythmias when indicated.
Hypersensitivity and idiosyncratic reactions
- True allergy to amide local anesthetics is rare. Cross-reactivity within the amide class can occur but is uncommon [2,3].
- Methemoglobinemia is much more common with other local anesthetics (e.g., prilocaine); lidocaine-associated methemoglobinemia is rare [2,3].
RISK FACTORS FOR TOXICITY
- Hepatic dysfunction or reduced hepatic blood flow (e.g., heart failure, shock): reduced clearance → higher levels [1–3].
- Older age: greater sensitivity and reduced clearance [1–3].
- Prolonged infusion: accumulation of active metabolites (MEGX, GX) that heighten CNS toxicity risk [2,3].
- Drug interactions: CYP1A2/3A4 inhibitors reduce clearance (e.g., cimetidine; certain macrolides and azole antifungals; amiodarone can increase lidocaine levels); beta blockers with high hepatic first-pass effect can reduce hepatic blood flow and clearance [2,3].
- Renal impairment: limited effect on parent drug but allows metabolite accumulation with prolonged therapy [1–3].
- Hypoxemia and acidosis: lower seizure threshold [2,3].
CONTRAINDICATIONS AND PRECAUTIONS
Contraindications
- Significant sinoatrial, atrioventricular, or intraventricular conduction block without a pacemaker [2,3].
- Known hypersensitivity to lidocaine or other amide-type local anesthetics [2,3].
Use with caution
- Hepatic impairment, heart failure, shock (reduce dose; monitor closely) [1–3].
- Seizure disorders: lidocaine lowers seizure threshold; titrate with care [2,3].
- Pregnancy and lactation: Widely used in obstetrics as a local anesthetic; for antiarrhythmic use, benefits should outweigh risks. Lidocaine crosses the placenta; clinically significant fetal adverse effects are uncommon at therapeutic doses. Small amounts enter breast milk; usually compatible with breastfeeding [1–3].
- Elderly: reduce maintenance doses; close monitoring for neurotoxicity [1–3].
DRUG INTERACTIONS YOU WILL ACTUALLY SEE
- CYP inhibitors reduce clearance and increase levels:
- Cimetidine, macrolides (e.g., erythromycin, clarithromycin), azole antifungals, certain SSRIs, amiodarone [2,3].
- Beta blockers (especially propranolol) can reduce hepatic blood flow and lidocaine clearance [2,3].
- Enzyme inducers (e.g., rifampin, chronic phenytoin) can increase clearance [2,3].
- Other depressants of cardiac conduction or negative inotropes: additive effects on conduction or hypotension are possible; monitor ECG and blood pressure [2,3].
PLACE IN THERAPY: HOW DOES IT COMPARE?
Compared with amiodarone
- Amiodarone is commonly used first for refractory VT/VF in cardiac arrest and for many ventricular tachyarrhythmias because of broad-spectrum efficacy and lower proarrhythmia risk than some legacy agents [2,3].
- Lidocaine’s advantages: rapid onset, ischemia-selective ventricular action, minimal hemodynamic depression, relatively clean conduction profile in normal tissue, few long-term toxicities (since use is short-term). Disadvantages: limited efficacy for atrial arrhythmias, short half-life requiring continuous infusion, and neurologic adverse effects with accumulation [1–3].
Compared with procainamide
- Procainamide (Class 1A) can be effective for stable monomorphic VT but more often depresses blood pressure and prolongs QRS/QT; lidocaine may be preferred in hypotensive or ischemic patients needing minimal hemodynamic impact [2,3].
Compared with mexiletine
- Mexiletine is the oral analog of lidocaine used for chronic suppression of ventricular arrhythmias in selected patients, and for certain channelopathies or neuropathic pain syndromes. Lidocaine is for acute IV therapy; mexiletine can be considered for maintenance in carefully selected cases, often under specialist care [2,3].
CONTROVERSIES AND EVIDENCE SNAPSHOT
- Prophylaxis post-MI: Historical trials showed reduced VF but increased asystole and no survival benefit; thus no routine prophylaxis to suppress PVCs after MI [1–3].
- In cardiac arrest algorithms, amiodarone is typically preferred, but lidocaine remains an acceptable alternative, particularly where amiodarone is unavailable or contraindicated, and in systems that have long experience with lidocaine [2,3].
- For digitalis toxicity, the definitive therapy is digoxin-specific antibody fragments; lidocaine can bridge acute arrhythmia suppression while Fab is obtained and administered [1–3].
SPECIAL POPULATIONS AND PRACTICAL DOSING ADJUSTMENTS
Older adults
- Lower maintenance infusion rates (e.g., 0.5–2 mg/min). Monitor mental status; early signs of neurotoxicity can be subtle [1–3].
Hepatic dysfunction and low-flow states
- Reduce bolus and infusion; for example, start at 0.5–1 mg/kg bolus and infuse at 0.5–2 mg/min with frequent reassessment [1–3].
- If arrhythmia suppression is inadequate despite careful titration and neurotoxicity limits further dose escalation, consider an alternative antiarrhythmic [2,3].
Heart failure/shock
- Clearance is flow-limited; dose reduction is often needed. Lidocaine’s minimal inotropy makes it comparatively safer than some alternatives, but monitor closely for accumulation [1–3].
Renal impairment
- Parent drug clearance not significantly affected, but metabolite accumulation can potentiate CNS toxicity during prolonged infusion—use the lowest effective dose and reassess daily [1–3].
Obesity
- Loading dose: typically based on actual body weight to saturate the larger volume of distribution; many clinicians cap single bolus doses (for example, 100–120 mg) and observe the response before repeating [2,3].
- Maintenance: consider dosing closer to ideal or adjusted body weight and titrate to effect and tolerability, since clearance is hepatic and not proportionate to total body weight [2,3].
Pregnancy and lactation
- Extensive obstetric experience as a local anesthetic; for antiarrhythmic use, reserve for clear indications. Fetal exposure occurs, but serious adverse effects are uncommon at therapeutic levels. Compatible with breastfeeding in typical doses [1–3].
PERI-INFUSION CHECKLIST: HOW TO USE LIDOCAINE SAFELY AND EFFECTIVELY
Before you start
- Confirm indication: ischemic VT, refractory VF/VT arrest, digitalis-induced ventricular arrhythmia, or perioperative ventricular irritability [1–3].
- Baseline ECG; correct potassium and magnesium; ensure oxygenation and treat underlying ischemia.
- Review medications for CYP inhibitors/inducers and other conduction depressants.
During therapy
- Give an appropriately sized bolus; reassess rhythm and hemodynamics within minutes.
- Start infusion promptly; select a rate aligned with age, hepatic function, and hemodynamics.
- Continuous ECG and neurologic monitoring; watch for early CNS signs (numbness, tinnitus, dysarthria, confusion).
- If continuing beyond 24 hours, re-evaluate daily; consider checking a level if response or toxicity is unclear.
When to change course
- Persistently recurrent VT/VF despite adequate bolus and infusion: consider adding or switching to another agent (e.g., amiodarone, procainamide in stable VT) and parallel strategies (reperfusion, ablation).
- Neurotoxicity: stop or reduce infusion, treat symptoms, and obtain levels; consider an alternative antiarrhythmic.
FREQUENTLY ASKED QUESTIONS AND COMMON PITFALLS
Q: Why didn’t lidocaine terminate this patient’s atrial fibrillation?
- Lidocaine has minimal atrial effects; it’s not indicated for AF/AFlutter or most supraventricular tachycardias [1–3].
Q: My patient’s lidocaine level is 7 micrograms/mL, but they’re asymptomatic and the VT is controlled. Should I stop it?
- Consider reducing the infusion and monitoring closely. Total plasma levels can be misleading when AAG is high (e.g., post-MI). If neurologic symptoms are absent and the arrhythmia is controlled transiently, a cautious reduction rather than abrupt cessation may be reasonable while planning a longer-term strategy [1–3].
Q: The patient has heart failure and shock. Is lidocaine safe?
- It is often safer hemodynamically than some alternatives, but clearance is reduced; use lower doses and vigilant monitoring for CNS toxicity [1–3].
Q: Does lidocaine prevent VF after MI?
- It reduces the incidence of VF but has not improved survival and may increase asystole; therefore routine prophylaxis is not recommended [1–3].
Q: Can I give lidocaine endotracheally during a code?
- Current practice generally prioritizes IO/IV access. If ET dosing is used as a last resort, absorption is variable and doses differ from IV; follow local protocols [2,3].
Q: Is lidocaine useful in torsades de pointes?
- It has limited utility in classic torsades (a pause-dependent polymorphic VT in prolonged QT). Magnesium and overdrive pacing are preferred. Lidocaine may help if there’s an ischemic ventricular substrate without marked QT prolongation [2,3].
A MINI CASE TO TIE IT TOGETHER
A 67-year-old man with an anterior STEMI is in the ICU post-PCI. He develops runs of monomorphic VT at 150 bpm with hypotension to 85/50 mmHg. Amiodarone is not immediately available; the rhythm persists despite lidocaine 100 mg IV bolus.
What now?
- Administer an additional 0.5–0.75 mg/kg bolus (e.g., 50–75 mg) while preparing a lidocaine infusion at 2 mg/min, titrating to effect. Correct potassium and magnesium. Recheck underlying ischemia (patency, pain, ST segments). If VT persists or recurs, obtain amiodarone when available and consider synchronized cardioversion if the patient remains unstable. Monitor for neurotoxicity as infusion continues. Once stabilized, revisit the need for continued infusion versus transition to another strategy [1–3].
PRACTICAL PEARLS YOU’LL REMEMBER
- Think “ischemic ventricle”: lidocaine works best when sodium channels spend time in the inactivated state and the membrane is partially depolarized [1–3].
- IV bolus plus infusion: bolus fills the tank; infusion keeps it filled. Without the infusion, effect fades quickly [2,3].
- Watch the brain to protect the heart: earliest toxicity signals are neurologic, not conduction changes [1–3].
- If the code cart is out of amiodarone, don’t be shy with lidocaine in refractory VT/VF while you continue high-quality CPR and defibrillation—just remember to reduce the drip in older or sick livers [1–3].
- Digoxin-related VT? Lidocaine is a time-tested bridge while you arrange definitive therapy with digoxin-immune Fab and correct electrolytes [1–3].
SUMMARY
Lidocaine remains a nimble, targeted antiarrhythmic for ischemia-driven ventricular arrhythmias. Its pharmacology is as elegant as it is practical: fast on–off sodium channel blockade that spares normal conduction while quieting irritable ventricles. In a world where amiodarone often takes center stage, lidocaine is still a key understudy—particularly when speed, ischemic selectivity, and hemodynamic neutrality matter. Used thoughtfully—with appropriate dosing, attention to hepatic clearance, and vigilant monitoring for neurologic toxicity—lidocaine can be as relevant in modern critical care as it was in the early days of coronary care units.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics. 14th ed. New York: McGraw-Hill Education; 2023.
- Katzung BG. Basic & Clinical Pharmacology. 15th ed. New York: McGraw-Hill Education; 2021.
- Rang HP, Ritter JM, Flower RJ, Henderson G. Rang & Dale’s Pharmacology. 10th ed. London: Elsevier; 2021.






[…] IB: Lidocaine, Mexiletine, […]