📋 Table of Contents
- Introduction to Diuretics
- Nephron Physiology – A Quick Review
- Classification of Diuretics
- Carbonic Anhydrase Inhibitors
- Osmotic Diuretics
- Loop Diuretics
- Thiazide & Thiazide-Like Diuretics
- Potassium-Sparing Diuretics
- ADH Antagonists (Vaptans)
- Comparative Analysis
- Electrolyte Disturbances
- Clinical Applications & Guidelines
- Drug Interactions
- Special Populations
- Key Takeaways
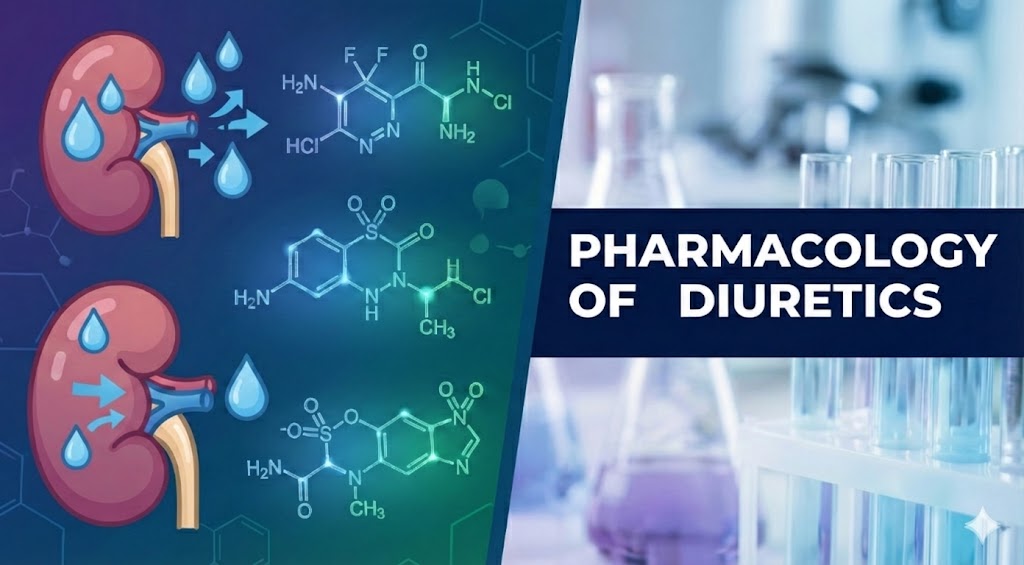
1. Introduction to Diuretics
Diuretics are a class of drugs that increase the rate of urine formation, thereby promoting the excretion of water and electrolytes (primarily sodium and chloride) from the body. They are among the most commonly prescribed medications worldwide, forming a cornerstone of therapy for hypertension, heart failure, edema, and numerous other conditions.
🔑 Key Concept
Diuretics work by inhibiting specific transport mechanisms in the renal tubules, reducing sodium reabsorption and increasing its excretion (natriuresis). Water follows sodium osmotically, leading to increased urine output (diuresis). Different classes act at different nephron segments, which determines their efficacy, electrolyte effects, and clinical applications.
The history of diuretics dates back to the 1930s when sulfanilamide was noted to cause metabolic acidosis and diuresis. This observation led to the development of carbonic anhydrase inhibitors, followed by thiazides in the 1950s, loop diuretics in the 1960s, and potassium-sparing agents. Today, diuretics remain first-line therapy for hypertension according to major guidelines.
📊 Why Are Diuretics Important?
- Hypertension affects ~1.3 billion people globally
- Heart failure affects 64 million people worldwide
- Edema is a common manifestation of liver, kidney, and heart disease
- Thiazides are recommended as first-line antihypertensives by JNC-8 and ESC/ESH
- Loop diuretics are essential for acute decompensated heart failure
⚠️ The Balancing Act
Diuretic therapy requires careful balance between achieving therapeutic fluid removal and avoiding electrolyte derangements. Overzealous diuresis can cause hypovolemia, electrolyte imbalances (hypokalemia, hyponatremia, hypomagnesemia), metabolic alkalosis or acidosis, and prerenal azotemia. Understanding the pharmacology of each class is essential for safe and effective use.
2. Nephron Physiology – A Quick Review
To understand how diuretics work, we must review the nephron’s transport mechanisms. The kidney filters ~180 L/day of plasma, reabsorbing ~99% of filtered sodium and water. Each nephron segment has distinct transporters that are targets for specific diuretic classes.
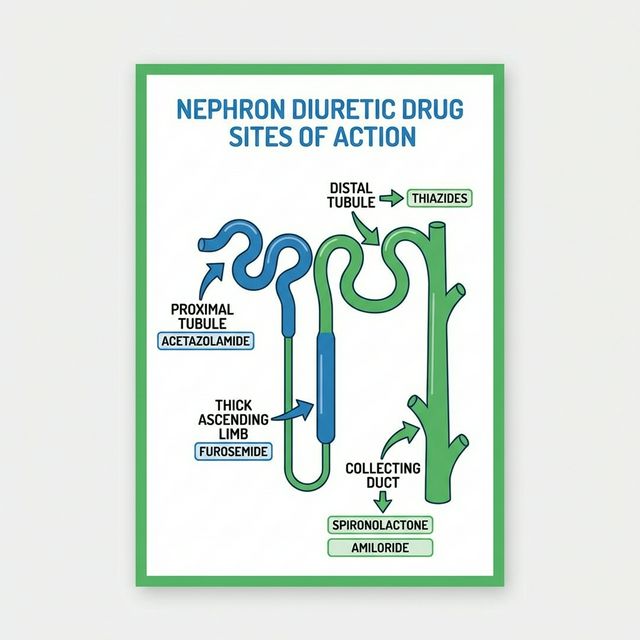
Figure 1: Nephron Diuretic Drug Sites of Action — Each class targets a specific transporter at a different nephron segment
The Nephron Segments & Their Transporters
Proximal Convoluted Tubule (PCT) – 65% Na⁺ reabsorption
Major site of NaHCO₃, glucose, amino acid, and phosphate reabsorption. Carbonic anhydrase (CA) catalyzes H⁺ secretion and HCO₃⁻ reabsorption. Also the site of action for osmotic diuretics.
Thick Ascending Limb of Loop of Henle (TAL) – 25% Na⁺
The Na⁺/K⁺/2Cl⁻ cotransporter (NKCC2) in the luminal membrane is the target of loop diuretics. This segment is impermeable to water, generating the medullary concentration gradient essential for urine concentration.
Distal Convoluted Tubule (DCT) – 5% Na⁺
The Na⁺/Cl⁻ cotransporter (NCC) is the target of thiazide diuretics. Also the site of active Ca²⁺ reabsorption (enhanced by thiazides via PTH-independent mechanisms).
Collecting Duct (CD) – 2-3% Na⁺
Epithelial sodium channel (ENaC) in principal cells is regulated by aldosterone. The target for potassium-sparing diuretics (amiloride blocks ENaC; spironolactone blocks mineralocorticoid receptor). Also contains aquaporin-2 (AQP2) channels regulated by ADH/vasopressin.
🔄 Key Principle: Site Determines Efficacy
The more proximally a diuretic acts, the greater the natriuretic effect — but with important caveats. Proximally-acting diuretics (e.g., CAIs) have their effect blunted by downstream reabsorption. Loop diuretics are the most potent because the TAL handles 25% of Na⁺ reabsorption with limited downstream compensatory capacity. Distally-acting drugs (thiazides, K⁺-sparing) are less potent natriuretics but have unique therapeutic properties.
Clinical Pearl: The Countercurrent Mechanism
Loop diuretics abolish the corticomedullary osmotic gradient by blocking NKCC2 in the TAL. This not only causes massive natriuresis but also impairs the kidney’s ability to concentrate urine — leading to production of isotonic or dilute urine. This is why loop diuretics are effective even in patients with severely impaired renal function (unlike thiazides, which require adequate GFR to be effective).
3. Classification of Diuretics
| Class | Drugs | Site of Action | Efficacy (% Na⁺) |
|---|---|---|---|
| Carbonic Anhydrase Inhibitors | Acetazolamide, Dorzolamide, Brinzolamide | Proximal Convoluted Tubule | ~5% |
| Osmotic Diuretics | Mannitol, Glycerol, Isosorbide | PCT, Loop of Henle, Collecting Duct | Variable |
| Loop Diuretics | Furosemide, Bumetanide, Torsemide, Ethacrynic acid | Thick Ascending Limb (TAL) | ~25% |
| Thiazide Diuretics | Hydrochlorothiazide, Chlorthalidone, Indapamide, Metolazone | Distal Convoluted Tubule (DCT) | ~5% |
| Potassium-Sparing (ENaC blockers) | Amiloride, Triamterene | Collecting Duct (ENaC) | ~2% |
| Potassium-Sparing (Aldosterone Antagonists) | Spironolactone, Eplerenone, Finerenone | Collecting Duct (MR receptor) | ~2% |
| ADH Antagonists (Vaptans) | Tolvaptan, Conivaptan | Collecting Duct (V2 receptor) | Aquaretic |
4. Carbonic Anhydrase Inhibitors (CAIs)
Carbonic anhydrase inhibitors were the first modern diuretics, derived from observations about sulfonamide antibiotics causing metabolic acidosis and alkaline diuresis. Though weak diuretics, they have important non-diuretic clinical applications.
⚙️ Mechanism of Action
Acetazolamide inhibits carbonic anhydrase (CA) in the proximal tubule (luminal CA-IV and intracellular CA-II). This blocks the conversion of CO₂ + H₂O → H₂CO₃ → H⁺ + HCO₃⁻, reducing:
- H⁺ secretion into the tubular lumen → less Na⁺/H⁺ exchange → reduced Na⁺ reabsorption
- HCO₃⁻ reabsorption → alkaline urine + metabolic acidosis
- Downstream: reduced Na⁺ reabsorption (~5% of filtered load)
📋 Pharmacokinetics
- Route: Oral (well absorbed)
- Onset: 1-2 hours (oral); 2 min (IV)
- Duration: 8-12 hours
- Half-life: 6-9 hours
- Excretion: Renal (unchanged)
- Self-limiting: Effect wanes in 2-3 days due to metabolic acidosis
🏥 Clinical Uses
- Glaucoma — reduces aqueous humor production (topical: dorzolamide, brinzolamide)
- Acute mountain sickness (AMS) — prophylaxis & treatment
- Metabolic alkalosis — correction (e.g., post-diuretic)
- Epilepsy — adjunctive (especially absence seizures)
- Pseudotumor cerebri — reduces CSF production
- Urinary alkalinization — to enhance excretion of acidic drugs (aspirin, uric acid)
⚠️ Adverse Effects of CAIs
- Metabolic acidosis (hyperchloremic, non-anion gap) — limits chronic use
- Hypokalemia — increased Na⁺ delivery to CD → K⁺ secretion
- Renal stones — alkaline urine + ↓ citrate + calcium phosphate precipitation
- Paresthesias — tingling of extremities (common)
- Drowsiness and malaise
- Sulfonamide allergy — contraindicated if allergic (all CAIs have sulfonamide moiety)
- Hepatic encephalopathy — in cirrhosis (↓ urinary NH₄⁺ excretion → ↑ blood ammonia)
Clinical Pearl: Why CAIs Are Weak Diuretics
Although the PCT reabsorbs 65% of filtered Na⁺, CAIs only block ~5% because: (1) most Na⁺ in the PCT is reabsorbed via mechanisms independent of carbonic anhydrase; (2) Na⁺ that escapes PCT reabsorption is recaptured by downstream segments (TAL and DCT); and (3) the resulting metabolic acidosis reduces HCO₃⁻ filtration, creating a self-limiting effect within 2-3 days.
5. Osmotic Diuretics
Osmotic diuretics are pharmacologically inert substances that are freely filtered at the glomerulus but poorly reabsorbed by the renal tubules. Their osmotic effect holds water within the tubular lumen, preventing reabsorption.
⚙️ Mechanism of Action
Mannitol (the prototype) is an inert sugar alcohol that increases tubular fluid osmolarity. It acts primarily in the PCT and descending limb of Loop of Henle (water-permeable segments). Key effects:
- Retains water in the tubular lumen → increased urine volume
- Extracts water from intracellular compartments → expands plasma volume transiently
- Reduces brain volume and intraocular pressure (major clinical applications)
- Washes out medullary concentration gradient
📋 Pharmacokinetics
- Route: IV only (not absorbed orally)
- Onset: 15-30 minutes
- Duration: 4-6 hours
- Distribution: Extracellular fluid
- Metabolism: Not metabolized
- Excretion: Renal (completely filtered, not reabsorbed)
🏥 Clinical Uses
- Raised intracranial pressure (ICP) — cerebral edema, neurosurgery
- Acute glaucoma — reduces intraocular pressure (IOP)
- Acute renal failure (prevention) — maintains tubular flow
- Dialysis disequilibrium syndrome
- Forced diuresis — in some poisonings
⚠️ Adverse Effects & Contraindications
- Pulmonary edema — initial plasma expansion can precipitate CHF
- Hyponatremia — dilutional (water extraction from cells)
- Hyperkalemia — water extraction from cells drags K⁺ out
- Dehydration — if fluid not replaced
- Contraindicated: Anuria (established renal failure), severe CHF, pulmonary congestion, active intracranial bleeding
Clinical Pearl: Mannitol Test Dose
Before giving full-dose mannitol in oliguric patients, a test dose (12.5 g IV) is administered. If urine output exceeds 30-50 mL/hr over the next 2-3 hours, the kidneys are responsive and full dosing can proceed. If no response, mannitol will accumulate in the plasma, causing dangerous volume expansion.
6. Loop Diuretics (High-Ceiling Diuretics)
Loop diuretics are the most potent diuretics available, capable of excreting up to 25% of the filtered sodium load. They act on the thick ascending limb (TAL) of the Loop of Henle and are indispensable in managing acute pulmonary edema, severe heart failure, and refractory edema.
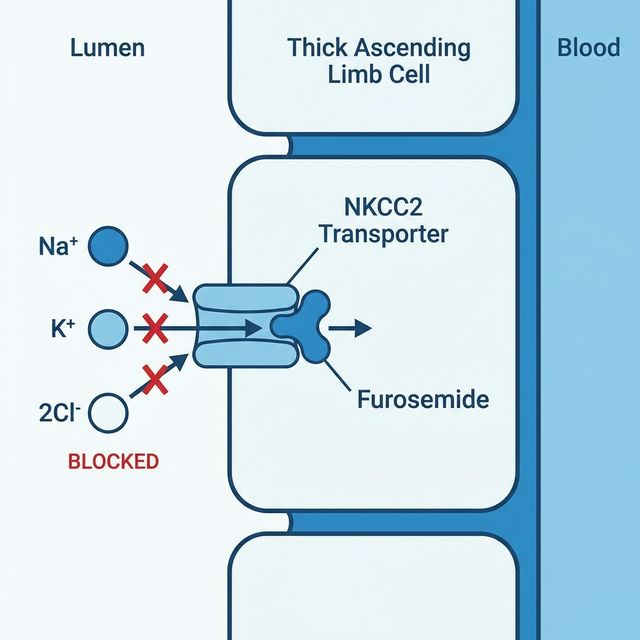
Figure 2: Loop Diuretic Mechanism of Action — Furosemide blocks the NKCC2 transporter in the Thick Ascending Limb, preventing Na⁺/K⁺/2Cl⁻ reabsorption
⚙️ Mechanism of Action
Loop diuretics inhibit the Na⁺/K⁺/2Cl⁻ cotransporter (NKCC2) on the luminal membrane of the TAL by competing for the Cl⁻ binding site. This causes:
- Massive natriuresis — blocks reabsorption of ~25% of filtered Na⁺
- Loss of K⁺, Cl⁻, Ca²⁺, Mg²⁺ — all depend on TAL transport
- Abolishes medullary concentration gradient → dilute urine
- ↑ Renal prostaglandin synthesis → renal vasodilation → ↑ RBF (partially blocked by NSAIDs)
- Venodilation — rapid IV furosemide reduces preload before diuresis begins (PGE₂/PGI₂-mediated)
| Drug | Potency | Bioavail. | Half-life | Duration | Key Notes |
|---|---|---|---|---|---|
| Furosemide (Lasix®) | 1x (reference) | 40-60% | 1.5-2 hrs | 4-6 hrs | Most commonly used; variable oral absorption |
| Bumetanide (Bumex®) | 40x furosemide | 80-100% | 1-1.5 hrs | 4-6 hrs | Better oral absorption; preferred if furosemide response poor |
| Torsemide (Demadex®) | 3x furosemide | 80-100% | 3-4 hrs | 6-8 hrs | Longest acting; hepatic metabolism; best bioavailability |
| Ethacrynic acid | ~1x furosemide | Variable | 1 hr | 4-6 hrs | Non-sulfonamide — safe in sulfa allergy; most ototoxic |
🏥 Clinical Uses
- Acute pulmonary edema — IV furosemide is first-line
- Congestive heart failure (CHF) — decongestion
- Chronic kidney disease — effective even at low GFR
- Nephrotic syndrome — severe edema
- Acute hypercalcemia — with saline hydration
- Hyperkalemia — emergency management (adjunct)
- Cerebral/pulmonary edema
- Ascites — in combination with spironolactone
⚠️ Adverse Effects
- Hypokalemia — ↑ Na⁺ delivery to CD → K⁺ secretion
- Metabolic alkalosis (contraction alkalosis)
- Hyponatremia, Hypomagnesemia
- Hypocalcemia — unlike thiazides!
- Ototoxicity — especially with IV bolus, aminoglycosides
- Hyperuricemia → gout
- Hyperglycemia (mild)
- Hypovolemia / Prerenal azotemia
- Sulfonamide allergy (except ethacrynic acid)
Clinical Pearl: Diuretic Resistance
Chronic loop diuretic use causes “braking phenomenon” — reduced effectiveness over time due to: (1) post-diuretic Na⁺ retention; (2) hypertrophy of DCT cells with upregulated NCC (distal nephron remodeling); (3) neurohormonal activation (RAAS, sympathetic). Solutions include: adding a thiazide (sequential nephron blockade), using continuous IV infusion, sodium restriction, and treating the underlying cause. The combination of loop + thiazide diuretic is synergistic but can cause profound electrolyte depletion.
🔑 Furosemide vs Torsemide
Furosemide has variable oral bioavailability (40-60%) that worsens in heart failure due to gut edema. Torsemide has consistent >80% bioavailability regardless of edema status, longer half-life, and anti-aldosterone properties. The TRANSFORM-HF trial showed no mortality difference, but torsemide is increasingly preferred for its pharmacokinetic advantages.
7. Thiazide & Thiazide-Like Diuretics
Thiazide diuretics are the most widely prescribed class of diuretics, primarily for hypertension. Despite being less potent natriuretics than loop diuretics, their sustained action and additional vascular effects make them ideal antihypertensive agents. They are recommended as first-line therapy for hypertension by JNC-8, ESC/ESH, and NICE guidelines.
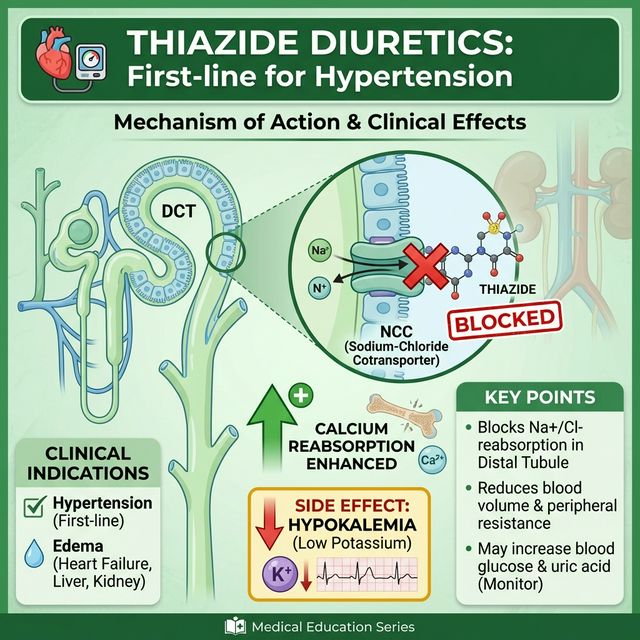
Figure 3: Thiazide Diuretics — Mechanism of Action & Clinical Effects. Blocks NCC in DCT, enhances calcium reabsorption, first-line for hypertension
⚙️ Mechanism of Action
Thiazides inhibit the Na⁺/Cl⁻ cotransporter (NCC) on the luminal membrane of the early distal convoluted tubule (DCT). This blocks ~5% of filtered Na⁺ reabsorption. Additional mechanisms:
- Short-term: ↓ Blood volume → ↓ cardiac output → ↓ BP
- Long-term (6-8 weeks): ↓ Peripheral vascular resistance (PVR) — the primary sustained antihypertensive mechanism. Volume returns to near-normal.
- ↑ Calcium reabsorption — enhances proximal Ca²⁺ reabsorption (useful in osteoporosis, hypocalcemia, calcium nephrolithiasis)
- Weak carbonic anhydrase inhibition (minor effect)
| Drug | Type | Half-life | Duration | Key Features |
|---|---|---|---|---|
| Hydrochlorothiazide (HCTZ) | Thiazide | 6-15 hrs | 12-16 hrs | Most commonly used; less effective than chlorthalidone for BP reduction |
| Chlorthalidone | Thiazide-like | 40-60 hrs | 48-72 hrs | Longer acting; stronger evidence for CV outcome reduction (ALLHAT trial); preferred by many guidelines |
| Indapamide | Thiazide-like | 14-18 hrs | 24-36 hrs | Direct vasodilator effect; less metabolic side effects; effective in CKD |
| Metolazone | Thiazide-like | 14 hrs | 12-24 hrs | Effective in renal impairment; potent when combined with loop diuretics (sequential nephron blockade) |
⚠️ Adverse Effects of Thiazides — “HyperGLUC”
Remember the mnemonic “HyperGLUC” for metabolic side effects:
- Hyperglycemia — impaired insulin release (hypokalemia-mediated)
- Hyperlipidemia — ↑ LDL, ↑ triglycerides (dose-dependent, reversible)
- Hyperuricemia — competes with uric acid secretion in PCT → gout
- Hypercalcemia — ↑ Ca²⁺ reabsorption (opposite to loop diuretics!)
Additional adverse effects:
- Hypokalemia — most common; ↑ Na⁺ delivery to CD → K⁺ secretion
- Hyponatremia — can be severe, especially in elderly women; impairs diluting capacity
- Hypomagnesemia
- Metabolic alkalosis (contraction + H⁺/K⁺ exchange)
- Sexual dysfunction — impotence (dose-dependent)
- Photosensitivity
- Sulfonamide allergy cross-reactivity
Clinical Pearl: Chlorthalidone vs Hydrochlorothiazide
Although HCTZ is more widely prescribed, chlorthalidone has stronger evidence for cardiovascular outcome reduction. Key differences: (1) Chlorthalidone has a much longer half-life (40-60 hrs vs 6-15 hrs), providing more consistent 24-hour BP control; (2) Chlorthalidone is 1.5-2x more potent per mg than HCTZ; (3) The landmark ALLHAT trial used chlorthalidone, not HCTZ. Many experts now recommend chlorthalidone as the preferred thiazide-type diuretic for hypertension.
✅ Unique Benefit: Calcium-Sparing Effect
Thiazides increase calcium reabsorption in the DCT (via indirect effects on the Na⁺/Ca²⁺ exchanger). This makes them useful for: (1) preventing calcium kidney stones in idiopathic hypercalciuria; (2) reducing osteoporosis risk in postmenopausal women; (3) treating nephrogenic diabetes insipidus (paradoxical antidiuretic effect — reduces urine volume by 40-50%). Remember: Loop diuretics WASTE calcium; Thiazides SAVE calcium.
8. Potassium-Sparing Diuretics
Potassium-sparing diuretics are weak natriuretics (~2-3% of filtered Na⁺) but are clinically important because they prevent potassium loss and have unique indications. They are divided into two subgroups based on mechanism of action.
🔹 ENaC Blockers: Amiloride & Triamterene
Mechanism: Directly block the epithelial sodium channel (ENaC) in principal cells of the collecting duct, independent of aldosterone. This reduces Na⁺ reabsorption and the electrical driving force for K⁺ and H⁺ secretion.
- Amiloride: Onset 2 hrs; duration 24 hrs; renally excreted unchanged — avoid in renal failure
- Triamterene: Hepatically metabolized; may cause renal stones (crystalluria)
- Used mainly as adjuncts to thiazides/loops to prevent hypokalemia
- Amiloride special use: Treatment of Liddle syndrome (gain-of-function ENaC mutation)
- Amiloride for lithium-induced NDI: Blocks lithium entry via ENaC
🔸 Aldosterone Antagonists: Spironolactone & Eplerenone
Mechanism: Competitive antagonists of the mineralocorticoid receptor (MR) in principal cells. Block aldosterone-mediated upregulation of ENaC and Na⁺/K⁺-ATPase, reducing Na⁺ reabsorption and K⁺ secretion.
- Spironolactone: Non-selective (also blocks androgen & progesterone receptors); active metabolite canrenone; t½ 1.4 hrs (canrenone: 16 hrs)
- Eplerenone: Selective MR antagonist — fewer endocrine side effects; t½ 4-6 hrs
- Finerenone: Non-steroidal MR antagonist; newer; shown to slow CKD progression in DKD (FIDELIO-DKD trial)
- Onset of spironolactone: 2-3 days (requires protein synthesis changes) — slow onset!
| Feature | Amiloride | Spironolactone | Eplerenone |
|---|---|---|---|
| Mechanism | Direct ENaC block | MR antagonist (non-selective) | MR antagonist (selective) |
| Aldosterone-dependent? | No | Yes | Yes |
| Anti-androgenic | No | Yes — gynecomastia, menstrual irregularities | Minimal |
| Key HF trial | — | RALES (35% ↓ mortality in NYHA III-IV) | EPHESUS, EMPHASIS-HF |
| Cost | Low | Low | Higher |
🏥 Clinical Uses of Aldosterone Antagonists
- Heart failure (HFrEF) — mortality reduction (RALES, EMPHASIS-HF trials). Guideline-directed therapy for EF ≤35%
- Primary hyperaldosteronism (Conn’s syndrome) — diagnostic and therapeutic
- Cirrhotic ascites — spironolactone is first-line (hyperaldosteronism drives ascites)
- Resistant hypertension — add-on 4th agent (often very effective)
- Polycystic ovary syndrome (PCOS) — spironolactone for hirsutism (anti-androgen effect)
- Acne — spironolactone for hormonal acne in women
- Diabetic kidney disease — finerenone (FIDELIO-DKD, FIGARO-DKD trials)
⚠️ DANGER: Hyperkalemia
The most serious adverse effect of ALL potassium-sparing diuretics is life-threatening hyperkalemia. Risk factors include:
- Renal impairment (CrCl <30 mL/min)
- Concurrent use of ACE inhibitors, ARBs, or K⁺ supplements
- Diabetes mellitus (hyporeninemic hypoaldosteronism)
- Elderly patients
Monitor serum K⁺ within 1 week of starting and regularly thereafter. Never combine two potassium-sparing diuretics. Avoid K⁺ supplements unless proven hypokalemic.
Clinical Pearl: Spironolactone’s Endocrine Side Effects
Spironolactone’s non-selectivity causes anti-androgenic effects: gynecomastia (up to 10%), breast tenderness, menstrual irregularities, and decreased libido. In the RALES trial, gynecomastia occurred in ~10% of men. Eplerenone was developed to avoid these effects — it has 500-fold less affinity for androgen receptors. For heart failure, eplerenone is preferred when gynecomastia is a concern, though spironolactone remains preferred for ascites (stronger evidence and lower cost).
9. ADH Antagonists (Vaptans)
Vaptans are a newer class of diuretics that block vasopressin (ADH) receptors, causing excretion of solute-free water (aquaresis) without significant electrolyte loss. They are unique because they increase serum sodium rather than decrease it.
⚙️ Mechanism & Drugs
- Tolvaptan: Selective V2 receptor antagonist (oral). Blocks AQP2 insertion in collecting duct → water excretion
- Conivaptan: V1a + V2 antagonist (IV). Also causes vasodilation via V1a blockade
- Result: Aquaresis — excretion of dilute, electrolyte-free urine
🏥 Clinical Uses
- Euvolemic hyponatremia — SIADH (primary indication)
- Hypervolemic hyponatremia — heart failure, cirrhosis
- Autosomal dominant polycystic kidney disease (ADPKD) — tolvaptan slows cyst growth (TEMPO 3:4 trial)
- NOT for hypovolemic hyponatremia — needs volume first
⚠️ Critical Warning: Osmotic Demyelination Syndrome (ODS)
Overly rapid correction of hyponatremia with vaptans can cause osmotic demyelination syndrome (central pontine myelinolysis). Must correct Na⁺ by no more than 8-10 mEq/L in the first 24 hours. Tolvaptan carries a boxed warning for hepatotoxicity — monitor liver function. Must be initiated in a hospital setting with close Na⁺ monitoring.
10. Comparative Analysis
| Feature | Loop | Thiazide | K⁺-Sparing | CAI |
|---|---|---|---|---|
| Site | TAL | DCT | CD | PCT |
| Efficacy | High (~25%) | Moderate (~5%) | Low (~2%) | Low (~5%) |
| K⁺ effect | ↓↓ Hypokalemia | ↓↓ Hypokalemia | ↑ Hyperkalemia | ↓ Hypokalemia |
| Ca²⁺ effect | ↓ Hypocalcemia | ↑ Hypercalcemia | No effect | No effect |
| Acid-base | Met. alkalosis | Met. alkalosis | Met. acidosis | Met. acidosis |
| Uric acid | ↑ Hyperuricemia | ↑ Hyperuricemia | No effect | No effect |
| Glucose | ↑ (mild) | ↑ Hyperglycemia | No effect | No effect |
| Works in CKD? | ✅ Yes | ❌ No (GFR <30)* | ❌ Avoid | ❌ No |
| Primary use | Edema, CHF, CKD | Hypertension | Adjunct, HF, ascites | Glaucoma, AMS |
*Exception: Metolazone and indapamide may retain some efficacy in moderate CKD
11. Electrolyte Disturbances
Critical Electrolyte Effects to Remember
Electrolyte derangements are the most common adverse effects of diuretics and the most commonly tested topic in pharmacology exams:
🔻 Hypokalemia (Loop & Thiazides)
Both loop and thiazide diuretics increase Na⁺ delivery to the collecting duct, where Na⁺ is reabsorbed via ENaC, creating a lumen-negative potential that drives K⁺ secretion. Also, volume depletion activates RAAS → aldosterone → more K⁺ loss. Monitor K⁺ and supplement or add K⁺-sparing agent.
🔻 Hyponatremia (Thiazides > Loop)
Thiazides impair urinary diluting capacity (block NCC in diluting segment) while preserving concentrating ability. This allows ADH-driven water retention with continued Na⁺ loss. Most dangerous in elderly women. Loop diuretics impair both diluting AND concentrating — paradoxically less hyponatremia risk.
🔄 Calcium: Loops vs Thiazides
Loop diuretics → hypocalcemia: Block NKCC2 → lose lumen-positive potential → reduced paracellular Ca²⁺ reabsorption. Thiazides → hypercalcemia: ↓ intracellular Na⁺ → enhanced basolateral Na⁺/Ca²⁺ exchange → ↑ Ca²⁺ reabsorption. Mnemonic: “Loops Lose calcium, Thiazides Trap calcium.”
⚖️ Acid-Base Effects
Metabolic alkalosis (loops/thiazides): Contraction alkalosis + ↑ H⁺ secretion in CD + ↑ HCO₃⁻ reabsorption. Metabolic acidosis (CAIs/K⁺-sparing): CAIs → HCO₃⁻ wasting; K⁺-sparing → ↓ H⁺ secretion in CD (type 4 RTA-like).
12. Clinical Applications & Guidelines
🫀 Hypertension
Thiazide/thiazide-like diuretics are first-line (JNC-8, ESC/ESH). Chlorthalidone 12.5-25 mg or indapamide 1.25-2.5 mg preferred. ALLHAT trial showed chlorthalidone non-inferior to ACEi and CCB. Low-dose is key — 12.5-25 mg HCTZ gives most of the BP effect with fewer metabolic side effects.
❤️ Heart Failure
Loop diuretics: For decongestion in HFrEF and HFpEF. Spironolactone/eplerenone: Mortality reduction in HFrEF (guideline-directed medical therapy). Sequential nephron blockade: Add metolazone/HCTZ to loops for diuretic resistance. Standard ratio for ascites: furosemide 40 mg + spironolactone 100 mg (ratio maintained).
🧠 Cerebral Edema
Mannitol 20% (0.5-1 g/kg IV) is first-line for acute raised ICP. Hypertonic saline (3%) is an alternative. Effect in 15-30 min, lasts 4-6 hrs. Maintain serum osmolality <320 mOsm/kg. Furosemide may be added for synergistic effect.
🦴 Nephrolithiasis & Osteoporosis
Thiazides reduce urinary calcium excretion → prevent calcium-containing kidney stones in idiopathic hypercalciuria. Also reduce fracture risk. Indapamide 2.5 mg or HCTZ 25 mg daily. Contraindicated: use loops for hypercalcemia (they WASTE calcium).
13. Drug Interactions
| Interaction | Mechanism | Clinical Effect |
|---|---|---|
| NSAIDs + Any Diuretic | ↓ Renal PGE₂ → ↓ RBF, ↓ GFR, ↑ Na⁺ reabsorption | Blunted diuretic and antihypertensive effect; ↑ risk of AKI |
| Loop + Aminoglycosides | Additive ototoxicity (damage to cochlear hair cells) | Irreversible hearing loss — avoid combination |
| Digoxin + K⁺-wasting diuretics | Hypokalemia enhances digoxin binding to Na⁺/K⁺-ATPase | Digoxin toxicity — always monitor K⁺ and Mg²⁺ |
| ACEi/ARB + K⁺-sparing | Both retain K⁺ via different mechanisms | Severe hyperkalemia — monitor K⁺ closely |
| Lithium + Thiazides | ↓ Na⁺ → ↑ proximal Li⁺ reabsorption | Lithium toxicity — reduce dose or avoid |
| Corticosteroids + K⁺-wasting | Additive K⁺ loss (mineralocorticoid effect) | Severe hypokalemia |
Clinical Pearl: NSAIDs — The “Diuretic Killer”
NSAIDs are the most common cause of diuretic resistance in clinical practice. They inhibit renal prostaglandin synthesis, which reduces renal blood flow, GFR, and sodium excretion. This is especially important in heart failure patients on loop diuretics. COX-2 selective inhibitors have the same effect. Always ask about NSAID use when evaluating poor diuretic response!
14. Special Populations
🤰 Pregnancy
- Generally avoided — can reduce placental perfusion
- Thiazides: Category B but can cause neonatal thrombocytopenia, hyponatremia
- Loop diuretics: Used if severe heart failure/pulmonary edema in pregnancy
- Spironolactone: Contraindicated (anti-androgenic — risk of feminization of male fetus)
- Mannitol: May be used for acute raised ICP if needed
🧓 Elderly
- Increased risk of hyponatremia (especially with thiazides in elderly women)
- Increased risk of orthostatic hypotension and falls
- Start with low doses and titrate slowly
- Monitor electrolytes and renal function frequently
- Thiazides remain effective for hypertension in elderly (SHEP trial, HYVET trial)
🏥 Chronic Kidney Disease
- Thiazides: Ineffective when GFR <30 (exception: metolazone, chlorthalidone at higher doses)
- Loop diuretics: Remain effective; may need higher doses (ceiling dose concept)
- K⁺-sparing: Avoid or use extreme caution — high hyperkalemia risk
- Finerenone: Approved for DKD even in moderate CKD (with monitoring)
🫁 Cirrhosis & Ascites
- Spironolactone is the cornerstone (100-400 mg/day) — counteracts hyperaldosteronism
- Add furosemide in ratio 100:40 (spironolactone:furosemide) to maintain K⁺ balance
- Avoid excessive diuresis (>0.5 kg/day without peripheral edema, >1 kg/day with)
- Acetazolamide contraindicated — worsens hepatic encephalopathy (↓ NH₄⁺ excretion)
15. Key Takeaways
📚 Recommended Resources for Further Reading
- Goodman & Gilman’s Pharmacological Basis of Therapeutics — Diuretics Chapter
- Katzung Basic & Clinical Pharmacology — Diuretic Agents
- ACC/AHA Heart Failure Guidelines (2022 Update)
- JNC-8 / ESC/ESH Hypertension Guidelines
- KDIGO Guidelines for CKD Management
- Ellison DH. “Diuretic Therapy and Resistance in Congestive Heart Failure.” Cardiology. 2001
📋 Disclaimer: This article is intended for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult qualified healthcare professionals for clinical decision-making.
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.