1. Introduction to Cardiac Electrophysiology
Understanding antiarrhythmic drugs requires a foundational understanding of the cardiac action potential (AP) and the ion channels that govern it. Cardiac arrhythmia is defined as any abnormality in the site of origin of the cardiac impulse, its rate and regularity, or its conduction.
1.1 Types of Cardiac Cells & Action Potentials
There are two main types of electrical tissues in the heart, distinguished by their action potentials:
- Fast Response Cells (Non-Pacemaker): Found in atrial and ventricular myocytes and the His-Purkinje system. Their rapid depolarization is driven by sodium (Na+) influx.
- Slow Response Cells (Pacemaker): Found in the Sinoatrial (SA) node and Atrioventricular (AV) node. Their depolarization is slower and driven by calcium (Ca2+) influx. They exhibit automaticity (spontaneous depolarization).
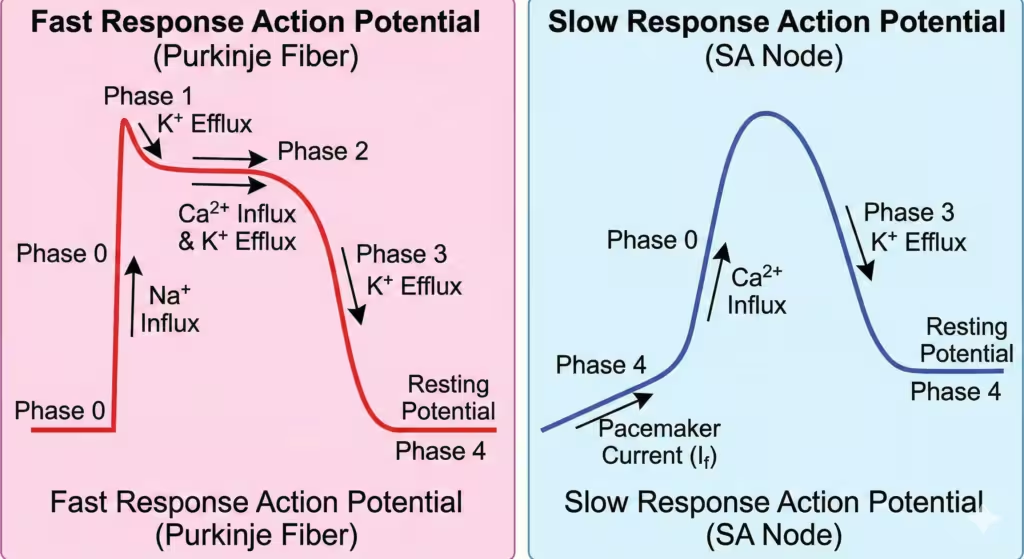
Figure 1. Comparison of Fast and Slow Response Action Potentials. The fast response AP (left) is characteristic of His-Purkinje fibers and myocytes, with a rapid Phase 0 driven by Na+ influx. The slow response AP (right) is characteristic of nodal tissue (SA, AV nodes), with a slower Phase 0 driven by Ca2+ influx and a spontaneous diastolic depolarization in Phase 4 driven by the pacemaker current (If).
1.2 The Cardiac Action Potential Phases
| Phase | Description | Major Drug Targets |
| Phase 0 | Rapid Depolarization (Na+ influx in fast cells, Ca2+ in slow cells) | Class I (Na+ blockers) Class IV (Ca2+ blockers – nodes) |
| Phase 1 | Early Repolarization (transient K+ efflux) | – |
| Phase 2 | Plateau (balance of Ca2+ influx and K+ efflux) | Class IV (minor effect) |
| Phase 3 | Rapid Repolarization (massive K+ efflux) | Class III (K+ blockers) |
| Phase 4 | Resting Potential (stable in fast cells, unstable in pacemakers) | Class II (β-blockers affect pacemaker slope) |
Key Concepts for Exams:
- Effective Refractory Period (ERP): The time during which the cell cannot be depolarized again by another impulse. Prolonging ERP is a key mechanism for stopping reentrant arrhythmias.
- State-Dependent Block: Many antiarrhythmics (especially Class I) bind more effectively to ion channels when they are in an “open” or “inactivated” state, rather than a “resting” state. Therefore, these drugs work better in rapidly firing tissues (tachycardia).
2. Mechanisms of Arrhythmogenesis
Arrhythmias arise from three fundamental mechanisms:
- Abnormal Automaticity:
- Enhanced Normal Automaticity: SA or AV node firing too fast due to sympathetic stimulation.
- Abnormal Automaticity: Non-pacemaker cells develop spontaneous depolarization.
- Triggered Activity (Afterdepolarizations):
- Secondary depolarizations triggered by a preceding AP, often due to intracellular Ca2+ overload (e.g., Digoxin toxicity).
- Reentry (Circus Movement):
- The most common mechanism for clinically significant arrhythmias (e.g., Atrial Fibrillation, VT post-MI, SVT).
- Requirements: A closed conduction loop, an area of unidirectional block, and slow conduction through the retrograde pathway so that the impulse arrives after the tissue is no longer refractory.
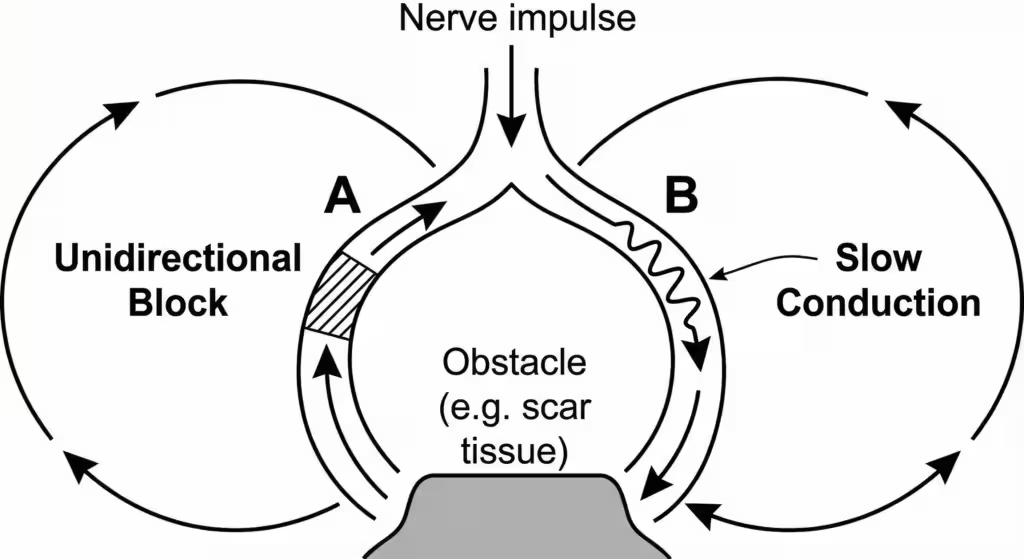
Figure 2. Mechanism of Reentry. An impulse travels down a pathway that bifurcates around an obstacle. Path A has a unidirectional block, preventing anterograde conduction. Path B has slow conduction. The impulse travels down Path B and then retrogradely up Path A, which is now no longer refractory. It then re-enters the circuit, establishing a continuous loop. Antiarrhythmic drugs work by either converting the unidirectional block to a bidirectional block or by prolonging the refractory period so the impulse finds the tissue unexcitable.
3. Classification of Antiarrhythmic Drugs
The Vaughan Williams Classification is the standard system used in pharmacology, classifying drugs based on their primary effect on ion channels and the action potential.
Note: This system has limitations as many drugs have multiple actions (e.g., Amiodarone spans all four classes).
| Class | Primary Mechanism | Main Effect on AP | Examples |
| Class I | Na+ Channel Blockers | Slow Phase 0 depolarization | (Subdivided below) |
| Class II | Beta-Adrenergic Blockers | Sympatholytic; slow Phase 4 in nodes | Metoprolol, Propranolol, Esmolol |
| Class III | K+ Channel Blockers | Prolong Phase 3 repolarization (↑ APD and ERP) | Amiodarone, Sotalol, Dofetilide |
| Class IV | Ca2+ Channel Blockers | Slow Phase 0 in nodal tissue; slow conduction | Verapamil, Diltiazem (Non-DHPs) |
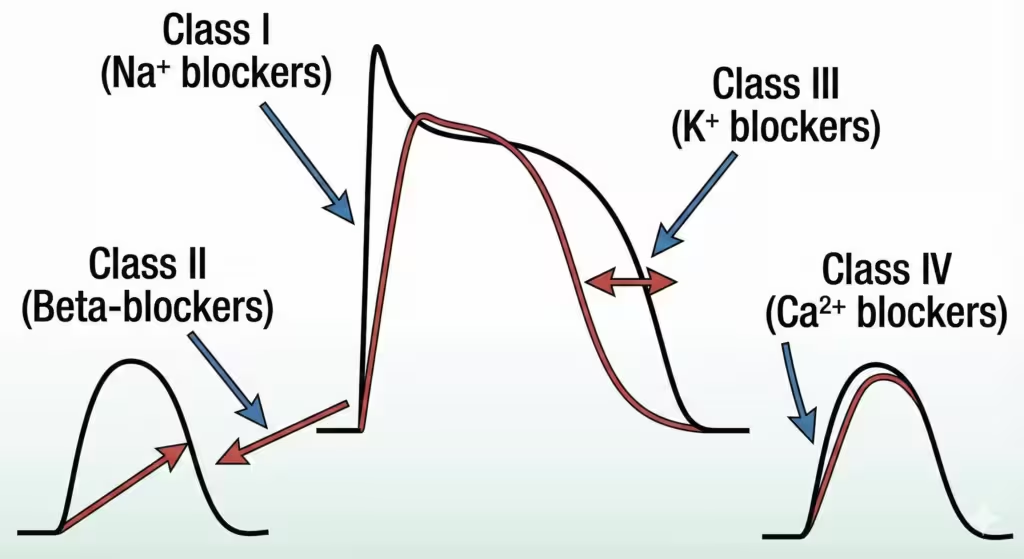
Figure 3. Effect of Antiarrhythmic Drug Classes on the Action Potential. Class I drugs decrease the slope of Phase 0 (Na+ influx). Class II drugs decrease the slope of Phase 4 depolarization in pacemakers. Class III drugs prolong Phase 3 repolarization (K+ efflux). Class IV drugs decrease the slope of Phase 0 in pacemaker cells (Ca2+ influx).
4. Class I: Sodium Channel Blockers
These drugs block voltage-gated fast Na+ channels, primarily affecting non-pacemaker tissue. They are subdivided into IA, IB, and IC based on the kinetics of channel binding and their effect on Action Potential Duration (APD).
4.1 Class IA: Moderate Na+ Blockers + K+ Block
- Drugs: Quinidine, Procainamide, Disopyramide.
- Mechanism: Moderate Na+ channel blockade (slows conduction) + K+ channel blockade (prolongs repolarization).
- ECG Effects: Widened QRS and prolonged QT interval.
- Toxicity: Quinidine causes “Cinchonism” and Torsades de Pointes (TdP). Procainamide causes drug-induced Lupus. Disopyramide has strong anticholinergic effects.
4.2 Class IB: Weak Na+ Blockers / Rapid Dissociation
- Drugs: Lidocaine, Mexiletine.
- Mechanism: Weak Na+ blockade with rapid kinetics. Shortens repolarization. Selectively affects ischemic tissue.
- Clinical Use: Lidocaine (IV) is the drug of choice for acute ventricular arrhythmias associated with myocardial infarction.
- Adverse Effects: CNS toxicity (drowsiness, seizures).
4.3 Class IC: Strong Na+ Blockers / Slow Dissociation
- Drugs: Flecainide, Propafenone.
- Mechanism: Marked Na+ blockade with slow kinetics. Little effect on repolarization. Drastically slows conduction.
- Clinical Use: “Pill-in-the-pocket” for paroxysmal Atrial Fibrillation in structurally normal hearts.
- Contraindication: Structural Heart Disease (ischemic heart disease, heart failure) due to high risk of fatal proarrhythmia (CAST Trial).
5. Class II: Beta-Adrenergic Blockers
- Drugs: Metoprolol, Propranolol, Esmolol (IV, ultra-short acting).
- Mechanism: Competitive antagonism of β1-receptors. Decreases sympathetic tone, depresses the slope of Phase 4 in nodes, and prolongs AV nodal conduction.
- Clinical Use: Rate control in Atrial Fibrillation/Flutter. Post-MI mortality reduction.
- Adverse Effects: Bradycardia, AV block, hypotension, bronchospasm.
6. Class III: Potassium Channel Blockers
- General Mechanism: Block repolarizing potassium channels (IKr), prolonging APD and ERP.
- ECG Effect: Prolongs the QT interval.
- Major Risk: All Class III agents carry a risk of inducing Torsades de Pointes (TdP).
6.1 Amiodarone: The “Broad Spectrum” Antiarrhythmic
Amiodarone is unique because it possesses characteristics of all four Vaughan Williams classes. It is highly effective for both supraventricular and ventricular arrhythmias and is preferred in heart failure patients.
Amiodarone Toxicity Profile (High Yield for PG Exams): Because of its iodine moiety, huge volume of distribution, and extremely long half-life (weeks), it causes multi-organ toxicity that requires careful monitoring.
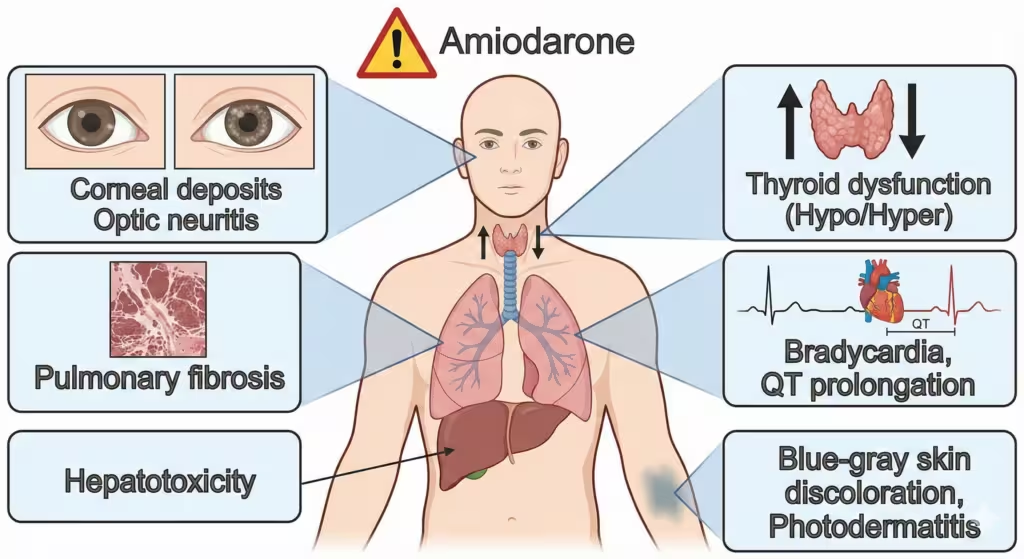
Figure 4. Amiodarone Toxicity Profile. Amiodarone can affect multiple organ systems. The most serious is pulmonary fibrosis. Other common side effects include thyroid dysfunction (hypo- or hyperthyroidism), corneal deposits, hepatotoxicity, bradycardia, QT prolongation, and blue-gray skin discoloration.
6.2 Other Class III Agents
- Sotalol: Non-selective β-blocker with potent Class III K+ blocking effects. High risk of TdP.
- Dofetilide: Pure Class III K+ blocker. Used for maintenance of sinus rhythm in AF. Requires inpatient initiation for QT monitoring.
7. Class IV: Calcium Channel Blockers (Non-DHP)
- Drugs: Verapamil, Diltiazem.
- Mechanism: Block L-type voltage-gated Ca2+ channels in slow-response tissues (SA and AV nodes). Slows conduction and increases refractoriness in the AV node.
- Clinical Use: Termination of paroxysmal SVT and rate control in AF.
- Contraindication: Decompensated Heart Failure (HFrEF) due to negative inotropic effects.
8. Miscellaneous Antiarrhythmic Drugs
8.1 Adenosine: The “Chemical Cardioverter”
- Mechanism: Activates A1 receptors in the AV node, causing transient, complete conduction block.
- Clinical Use: Drug of choice for terminating acute Paroxysmal Supraventricular Tachycardia (PSVT).
- Pharmacokinetics: Extremely short half-life (<10s). Must be given as a rapid IV bolus.
8.2 Digoxin
- Mechanism: Indirectly increases vagal tone, slowing conduction through the AV node.
- Clinical Use: Rate control in Atrial Fibrillation, especially in patients with heart failure.
8.3 Magnesium Sulfate
- Clinical Use: Drug of choice for Torsades de Pointes (TdP).
9. The “Proarrhythmic” Effect
A critical concept is that all antiarrhythmic drugs can cause arrhythmias.
- Torsades de Pointes (TdP): Caused by QT-prolonging drugs (Class IA, III).
- Incessant VT/VF: Class IC agents can cause fatal arrhythmias in diseased hearts (CAST trial).
10. Exam Summary Table: Clinical Applications
| Arrhythmia Clinical Scenario | Preferred Drugs | Drugs to AVOID |
| Acute PSVT (termination) | Adenosine (1st line), IV Verapamil/Diltiazem. | |
| Atrial Fibrillation (Rate Control) | β-blockers, Ca2+ Blockers (Non-DHP). | |
| Ventricular Tachycardia (Acute, Ischemic) | Lidocaine (IV), Amiodarone (IV). | Class IA/IC. |
| Torsades de Pointes (TdP) | IV Magnesium (1st line). | Any QT-prolonging drug (Class IA, III). |
| Arrhythmias in Heart Failure (HFrEF) | Amiodarone, β-blockers, Digoxin. | Non-DHP CCBs (Verapamil, Diltiazem), Class IC. |
11. References
- Brunton LL, Hilal-Dandan R, Knollmann BC. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics. 13th ed. New York: McGraw-Hill Education; 2018.
- Katzung BG. Basic & Clinical Pharmacology. 15th ed. New York: McGraw-Hill Education; 2021.
Quiz on antiarrhythmic drugs
📚 AI Pharma Quiz Generator
🎉 Quiz Results
Medical Disclaimer
The medical information on this post is for general educational purposes only and is provided by Pharmacology Mentor. While we strive to keep content current and accurate, Pharmacology Mentor makes no representations or warranties, express or implied, regarding the completeness, accuracy, reliability, suitability, or availability of the post, the website, or any information, products, services, or related graphics for any purpose. This content is not a substitute for professional medical advice, diagnosis, or treatment; always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition and never disregard or delay seeking professional advice because of something you have read here. Reliance on any information provided is solely at your own risk.